Childhood Nasopharyngeal Cancer Treatment (PDQ®)–Health Professional Version
Incidence
Nasopharyngeal carcinoma arises in the lining of the nasal cavity and pharynx, and it accounts for about one-third of all cancers of the upper airways in children.[1,2]
Nasopharyngeal carcinoma is exceedingly rare in children younger than 10 years.[3] The age-adjusted incidence rates (2016–2020) for both sexes and all races of children younger than 20 years in the United States are shown in Table 1.[3]
| Age | Rate per 1,000,000 |
|---|---|
| aAdapted from the National Childhood Cancer Registry.[3] | |
| Ages 0–4 years | 0 |
| Ages 5–9 years | 0.1 |
| Ages 10–14 years | 0.5 |
| Ages 15–19 years | 1.1 |
The incidence of nasopharyngeal carcinoma is characterized by racial and geographic variations, with an endemic distribution among well-defined ethnic groups. These groups include inhabitants of some areas in North Africa, the Mediterranean basin, and, particularly, Southeast Asia. In the United States, the incidence of nasopharyngeal carcinoma is markedly higher in Black children than in other racial or ethnic groups (see Table 2).[3–5]
| Race/Ethnicity | Rate per 1,000,000 | Lower 95% CI | Upper 95% CI |
|---|---|---|---|
| CI = confidence interval. | |||
| aAdapted from the National Childhood Cancer Registry.[3] | |||
| All races | 0.4 | 0.3 | 0.5 |
| Hispanic | 0.4 | 0.3 | 0.6 |
| Non-Hispanic Asian/Pacific Islander | 0.4 | 0.2 | 0.8 |
| Non-Hispanic Black | 1.0 | 0.7 | 1.4 |
| Non-Hispanic White | 0.2 | 0.2 | 0.3 |
References
- Ayan I, Kaytan E, Ayan N: Childhood nasopharyngeal carcinoma: from biology to treatment. Lancet Oncol 4 (1): 13-21, 2003. [PUBMED Abstract]
- Yan Z, Xia L, Huang Y, et al.: Nasopharyngeal carcinoma in children and adolescents in an endemic area: a report of 185 cases. Int J Pediatr Otorhinolaryngol 77 (9): 1454-60, 2013. [PUBMED Abstract]
- National Cancer Institute: NCCR*Explorer: An interactive website for NCCR cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed February 25, 2025.
- Sultan I, Casanova M, Ferrari A, et al.: Differential features of nasopharyngeal carcinoma in children and adults: a SEER study. Pediatr Blood Cancer 55 (2): 279-84, 2010. [PUBMED Abstract]
- Richards MK, Dahl JP, Gow K, et al.: Factors Associated With Mortality in Pediatric vs Adult Nasopharyngeal Carcinoma. JAMA Otolaryngol Head Neck Surg 142 (3): 217-22, 2016. [PUBMED Abstract]
Risk Factors
Epstein-Barr virus (EBV). Nasopharyngeal carcinoma is strongly associated with EBV infection. In addition to the serological evidence of infection in more than 98% of patients, EBV DNA is present as a monoclonal episome in the nasopharyngeal carcinoma cells, and tumor cells can have EBV antigens on their cell surface.[1] The circulating levels of EBV DNA and serological documentation of EBV infection may help with the diagnosis.[1]
HLA subtypes. Specific HLA subtypes, such as the HLA A2 Bsin2 haplotype, are associated with a higher risk of nasopharyngeal carcinoma.[1,2]
References
- Chen YP, Chan ATC, Le QT, et al.: Nasopharyngeal carcinoma. Lancet 394 (10192): 64-80, 2019. [PUBMED Abstract]
- Ayan I, Kaytan E, Ayan N: Childhood nasopharyngeal carcinoma: from biology to treatment. Lancet Oncol 4 (1): 13-21, 2003. [PUBMED Abstract]
Clinical Presentation
Given the rich lymphatic drainage of the nasopharynx, bilateral cervical lymphadenopathy is often the first sign of nasopharyngeal carcinoma. Other signs and symptoms include the following:[1,2]
- Nosebleeds.
- Nasal congestion and obstruction.
- Headache.
- Otalgia.
- Otitis media.
The tumor spreads locally to adjacent areas of the oropharynx and may invade the skull base, resulting in cranial nerve palsy or difficulty with movements of the jaw (trismus). Distant metastatic sites may include the bones, lungs, and liver.
References
- Yan Z, Xia L, Huang Y, et al.: Nasopharyngeal carcinoma in children and adolescents in an endemic area: a report of 185 cases. Int J Pediatr Otorhinolaryngol 77 (9): 1454-60, 2013. [PUBMED Abstract]
- Hu S, Xu X, Xu J, et al.: Prognostic factors and long-term outcomes of nasopharyngeal carcinoma in children and adolescents. Pediatr Blood Cancer 60 (7): 1122-7, 2013. [PUBMED Abstract]
Diagnostic and Staging Evaluation
Diagnostic tests determine the extent of the primary tumor and the presence of metastases. Visualization of the nasopharynx, by an otolaryngologist using nasal endoscopy and magnetic resonance imaging of the head and neck, can determine the extent of the primary tumor.
A diagnosis can be made from a biopsy of the primary tumor or enlarged lymph nodes of the neck. Nasopharyngeal carcinomas must be distinguished from all other cancers that can present with enlarged lymph nodes and from other types of cancer in the head and neck area. Thus, diseases such as thyroid cancer, rhabdomyosarcoma, non-Hodgkin lymphoma (including Burkitt lymphoma), and Hodgkin lymphoma must be considered, as well as benign conditions such as nasal angiofibroma, which usually presents with epistaxis in adolescent males, infectious lymphadenitis, and Rosai-Dorfman disease.
Evaluation of the chest and abdomen by computed tomography (CT) and bone scan is performed to determine whether there is metastatic disease. Fluorine F 18-fludeoxyglucose positron emission tomography (PET)–CT may also be helpful in the evaluation of potential metastatic lesions.[1]
References
- Cheuk DK, Sabin ND, Hossain M, et al.: PET/CT for staging and follow-up of pediatric nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging 39 (7): 1097-106, 2012. [PUBMED Abstract]
Histology
The World Health Organization (WHO) recognizes the following three histological subtypes of nasopharyngeal carcinoma:
- Type I: Keratinizing squamous cell carcinoma.
- Type II: Nonkeratinizing squamous cell carcinoma. Type II is further defined by the presence or absence of lymphoid infiltration as type IIa or IIb, respectively.
- Type III: Undifferentiated carcinoma. Type III is further defined by the presence or absence of lymphoid infiltration as type IIIa or IIIb, respectively.
Children with nasopharyngeal carcinoma are more likely to have WHO type II or type III disease.[1,2]
References
- Sultan I, Casanova M, Ferrari A, et al.: Differential features of nasopharyngeal carcinoma in children and adults: a SEER study. Pediatr Blood Cancer 55 (2): 279-84, 2010. [PUBMED Abstract]
- Richards MK, Dahl JP, Gow K, et al.: Factors Associated With Mortality in Pediatric vs Adult Nasopharyngeal Carcinoma. JAMA Otolaryngol Head Neck Surg 142 (3): 217-22, 2016. [PUBMED Abstract]
Genomics of Childhood Nasopharyngeal Carcinoma
Four tertiary academic medical centers in China studied 30 patients (25 male and 5 female) with pathologically confirmed nasopharyngeal carcinoma who were younger than 20 years.[1] Nasopharyngeal primary tumors with paired blood samples were collected and sequenced using whole-exome sequencing. Several genes such as SHOC1 (formerly known as C9orf84) (20%), ZFHX4 (16.7%), ZC3H6 (16.7%), and RBM38 (16.7%) were frequently altered in nasopharyngeal carcinoma. Copy number analysis revealed highly recurring gain/amplification of the HLA class II genes at 6p21.32 (63.3%) and losses of TOLLIP at 11p15.5 (20%).
In another analysis, homozygous deletion of the CDKN2A locus on 9p21.3 was confirmed in 7 of 15 nasopharyngeal carcinoma specimens (46.7%) and in 3 of 5 cell lines/patient-derived xenografts (60%). CCND1 amplification was found in 3 of 20 nasopharyngeal tumors (15%).[2] Whole-genome sequencing of nasopharyngeal carcinoma revealed that TP53 was the most significantly altered gene (n = 10), followed by TRAF3, NFKBIA, AEBP1, and NLRC5. All of these genes have been reported to regulate nuclear factor kappa B.[3] In addition, significant somatic aberrations detected in HLA-A and NLRC5 suggest the impairment of antigen presentation, while PTEN variants may activate the PI3K pathway. This study found four coding genes that were significantly altered, namely PLIN4, MUC21, SLC35G5, and ERVW-1.
References
- Wu B, Shen L, Peng G, et al.: Molecular characteristics of pediatric nasopharyngeal carcinoma using whole-exome sequencing. Oral Oncol 135: 106218, 2022. [PUBMED Abstract]
- Tsang CM, Lui VWY, Bruce JP, et al.: Translational genomics of nasopharyngeal cancer. Semin Cancer Biol 61: 84-100, 2020. [PUBMED Abstract]
- Bruce JP, To KF, Lui VWY, et al.: Whole-genome profiling of nasopharyngeal carcinoma reveals viral-host co-operation in inflammatory NF-κB activation and immune escape. Nat Commun 12 (1): 4193, 2021. [PUBMED Abstract]
Prognosis
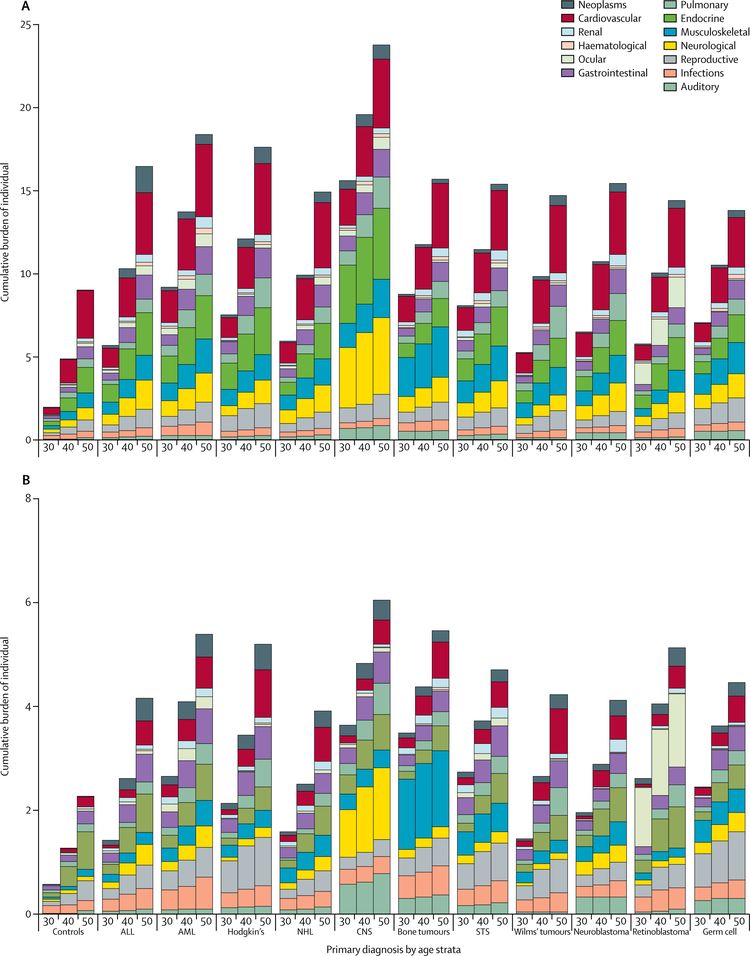
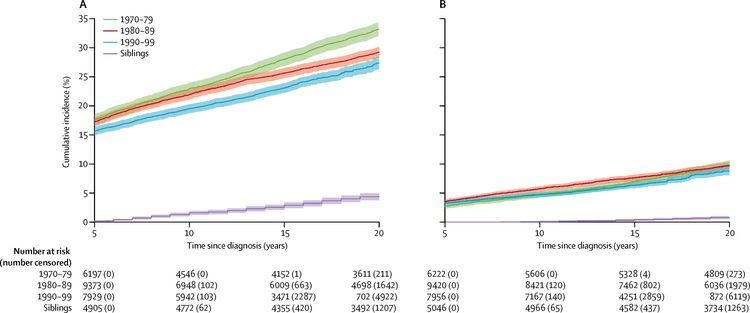
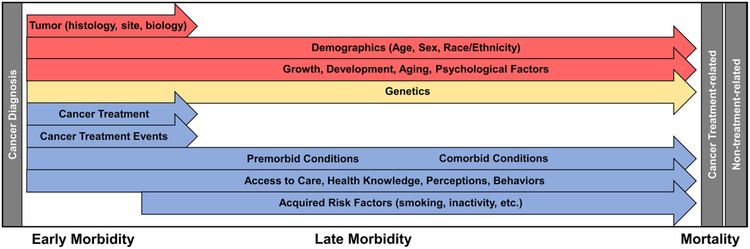
The overall survival of children and adolescents with nasopharyngeal carcinoma has improved over the last four decades through the use of state-of-the-art multimodal treatment.[1–8] The 5-year relative survival rate was 91% for children younger than 20 years who were diagnosed with nasopharyngeal carcinoma in the United States between 2013 and 2019.[9] After controlling for stage, children with nasopharyngeal carcinoma have significantly better outcomes than adults.[1,7] However, the intensive use of chemotherapy and radiation therapy results in significant acute and long-term morbidities, including subsequent neoplasms.[1–3,6]
References
- Sultan I, Casanova M, Ferrari A, et al.: Differential features of nasopharyngeal carcinoma in children and adults: a SEER study. Pediatr Blood Cancer 55 (2): 279-84, 2010. [PUBMED Abstract]
- Cheuk DK, Billups CA, Martin MG, et al.: Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117 (1): 197-206, 2011. [PUBMED Abstract]
- Casanova M, Bisogno G, Gandola L, et al.: A prospective protocol for nasopharyngeal carcinoma in children and adolescents: the Italian Rare Tumors in Pediatric Age (TREP) project. Cancer 118 (10): 2718-25, 2012. [PUBMED Abstract]
- Buehrlen M, Zwaan CM, Granzen B, et al.: Multimodal treatment, including interferon beta, of nasopharyngeal carcinoma in children and young adults: preliminary results from the prospective, multicenter study NPC-2003-GPOH/DCOG. Cancer 118 (19): 4892-900, 2012. [PUBMED Abstract]
- Hu S, Xu X, Xu J, et al.: Prognostic factors and long-term outcomes of nasopharyngeal carcinoma in children and adolescents. Pediatr Blood Cancer 60 (7): 1122-7, 2013. [PUBMED Abstract]
- Sahai P, Mohanti BK, Sharma A, et al.: Clinical outcome and morbidity in pediatric patients with nasopharyngeal cancer treated with chemoradiotherapy. Pediatr Blood Cancer 64 (2): 259-266, 2017. [PUBMED Abstract]
- Richards MK, Dahl JP, Gow K, et al.: Factors Associated With Mortality in Pediatric vs Adult Nasopharyngeal Carcinoma. JAMA Otolaryngol Head Neck Surg 142 (3): 217-22, 2016. [PUBMED Abstract]
- Gioacchini FM, Tulli M, Kaleci S, et al.: Prognostic aspects in the treatment of juvenile nasopharyngeal carcinoma: a systematic review. Eur Arch Otorhinolaryngol 274 (3): 1205-1214, 2017. [PUBMED Abstract]
- National Cancer Institute: NCCR*Explorer: An interactive website for NCCR cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed February 25, 2025.
Stage Information for Childhood Nasopharyngeal Carcinoma
Tumor staging is performed using the tumor-node-metastasis (TNM) classification system of the American Joint Committee on Cancer (AJCC).[1,2]
The AJCC has designated staging by TNM classification to define nasopharyngeal carcinoma.[3]
| Stage | TNM | Description |
|---|---|---|
| T = primary tumor; N = regional lymph node; M = distant metastasis. | ||
| aReprinted with permission from AJCC: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 103–11. | ||
| 0 | Tis, N0, M0 | Tis = Carcinoma in situ. |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| Stage | TNM | Description |
|---|---|---|
| T = primary tumor; N = regional lymph node; M = distant metastasis. | ||
| aReprinted with permission from AJCC: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 103–11. | ||
| I | T1, N0, M0 | T1 = Tumor confined to nasopharynx, or extension to oropharynx and/or nasal cavity without parapharyngeal involvement. |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| Stage | TNM | Description |
|---|---|---|
| T = primary tumor; N = regional lymph node; M = distant metastasis; EBV = Epstein-Barr virus. | ||
| aReprinted with permission from AJCC: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 103–11. | ||
| II | T0, Tis, T1, N1, M0 | T0 = No tumor identified, but EBV-positive cervical node(s) involvement. |
| Tis = Carcinoma in situ. | ||
| T1 = Tumor confined to nasopharynx, or extension to oropharynx and/or nasal cavity without parapharyngeal involvement. | ||
| N1 = Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| T2, N0, M0 | T2 = Tumor with extension to parapharyngeal space, and/or adjacent soft tissue involvement (medial pterygoid, lateral pterygoid, prevertebral muscles). | |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| T2, N1, M0 | T2 = Tumor with extension to parapharyngeal space, and/or adjacent soft tissue involvement (medial pterygoid, lateral pterygoid, prevertebral muscles). | |
| N1 = Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| Stage | TNM | Description |
|---|---|---|
| T = primary tumor; N = regional lymph node; M = distant metastasis; EBV = Epstein-Barr virus. | ||
| aReprinted with permission from AJCC: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 103–11. | ||
| III | T0, Tis, T1, N2, M0 | T0 = No tumor identified, but EBV-positive cervical node(s) involvement. |
| Tis = Carcinoma in situ. | ||
| T1 = Tumor confined to nasopharynx, or extension to oropharynx and/or nasal cavity without parapharyngeal involvement. | ||
| N2 = Bilateral metastasis in cervical lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| T2, N2, M0 | T2 = Tumor with extension to parapharyngeal space, and/or adjacent soft tissue involvement (medial pterygoid, lateral pterygoid, prevertebral muscles). | |
| N2 = Bilateral metastasis in cervical lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| T3, N0, M0 | T3 = Tumor with infiltration of bony structures at skull base, cervical vertebra, pterygoid structures, and/or paranasal sinuses. | |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| T3, N1, M0 | T3 = Tumor with infiltration of bony structures at skull base, cervical vertebra, pterygoid structures, and/or paranasal sinuses. | |
| N1 = Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| T3, N2, M0 | T3 = Tumor with infiltration of bony structures at skull base, cervical vertebra, pterygoid structures, and/or paranasal sinuses. | |
| N2 = Bilateral metastasis in cervical lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| Stage | TNM | Description |
|---|---|---|
| T = primary tumor; N = regional lymph node; M = distant metastasis; EBV = Epstein-Barr virus. | ||
| aReprinted with permission from AJCC: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 103–11. | ||
| IVA | T4, N0, M0 | T4 = Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotid gland, and/or extensive soft tissue infiltration beyond the lateral surface of the lateral pterygoid muscle. |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| T4, N1, M0 | T4 = Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotid gland, and/or extensive soft tissue infiltration beyond the lateral surface of the lateral pterygoid muscle. | |
| N1 = Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| T4, N2, M0 | T4 = Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotid gland, and/or extensive soft tissue infiltration beyond the lateral surface of the lateral pterygoid muscle. | |
| N2 = Bilateral metastasis in cervical lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| Any T, N3, M0 | TX = Primary tumor cannot be assessed. | |
| T0 = No tumor identified, but EBV-positive cervical node(s) involvement. | ||
| Tis = Carcinoma in situ. | ||
| T1 = Tumor confined to nasopharynx, or extension to oropharynx and/or nasal cavity without parapharyngeal involvement. | ||
| T2 = Tumor with extension to parapharyngeal space, and/or adjacent soft tissue involvement (medial pterygoid, lateral pterygoid, prevertebral muscles). | ||
| T3 = Tumor with infiltration of bony structures at skull base, cervical vertebra, pterygoid structures, and/or paranasal sinuses. | ||
| T4 = Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotid gland, and/or extensive soft tissue infiltration beyond the lateral surface of the lateral pterygoid muscle. | ||
| N3 = Unilateral or bilateral metastasis in cervical lymph node(s), >6 cm in greatest dimension, and/or extension below the caudal border of cricoid cartilage. | ||
| M0 = No distant metastasis. | ||
| IVB | Any T, Any N, M1 | Any T = See Stage IVA above. |
| NX = Regional lymph nodes cannot be assessed. | ||
| N0 = No regional lymph node metastasis. | ||
| N1 = Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| N2 = Bilateral metastasis in cervical lymph node(s), ≤6 cm in greatest dimension, above the caudal border of cricoid cartilage. | ||
| N3 = Unilateral or bilateral metastasis in cervical lymph node(s), >6 cm in greatest dimension, and/or extension below the caudal border of cricoid cartilage. | ||
| M1 = Distant metastasis. | ||
More than 90% of children and adolescents with nasopharyngeal carcinoma present with advanced disease (stage III/IV or T3/T4).[4,5] Population-based studies have reported that patients younger than 20 years had a higher incidence of advanced-stage disease than did adult patients.[6,7] However, less than 10% of children and adolescents with nasopharyngeal carcinoma presented with distant metastases at diagnosis.[4,5,8]
References
- Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. Springer; 2017.
- Lee AWM, Lydiatt WM, Colevas AD, et al.: Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. Springer; 2017, pp 103-11.
- Nasopharynx. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. Springer; 2017, pp. 103–11.
- Cheuk DK, Billups CA, Martin MG, et al.: Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117 (1): 197-206, 2011. [PUBMED Abstract]
- Casanova M, Bisogno G, Gandola L, et al.: A prospective protocol for nasopharyngeal carcinoma in children and adolescents: the Italian Rare Tumors in Pediatric Age (TREP) project. Cancer 118 (10): 2718-25, 2012. [PUBMED Abstract]
- Sultan I, Casanova M, Ferrari A, et al.: Differential features of nasopharyngeal carcinoma in children and adults: a SEER study. Pediatr Blood Cancer 55 (2): 279-84, 2010. [PUBMED Abstract]
- Richards MK, Dahl JP, Gow K, et al.: Factors Associated With Mortality in Pediatric vs Adult Nasopharyngeal Carcinoma. JAMA Otolaryngol Head Neck Surg 142 (3): 217-22, 2016. [PUBMED Abstract]
- Buehrlen M, Zwaan CM, Granzen B, et al.: Multimodal treatment, including interferon beta, of nasopharyngeal carcinoma in children and young adults: preliminary results from the prospective, multicenter study NPC-2003-GPOH/DCOG. Cancer 118 (19): 4892-900, 2012. [PUBMED Abstract]
Special Considerations for the Treatment of Children With Cancer
Cancer in children and adolescents is rare, although the overall incidence has slowly increased since 1975.[1] Children and adolescents with cancer should be referred to medical centers that have a multidisciplinary team of cancer specialists with experience treating the cancers that occur during childhood and adolescence. This multidisciplinary team approach incorporates the skills of the following pediatric specialists and others to ensure that children receive treatment, supportive care, and rehabilitation to achieve optimal survival and quality of life:
- Primary care physicians.
- Pediatric surgeons.
- Pathologists.
- Pediatric radiation oncologists.
- Pediatric medical oncologists and hematologists.
- Ophthalmologists.
- Rehabilitation specialists.
- Pediatric oncology nurses.
- Social workers.
- Child-life professionals.
- Psychologists.
- Nutritionists.
For specific information about supportive care for children and adolescents with cancer, see the summaries on Supportive and Palliative Care.
The American Academy of Pediatrics has outlined guidelines for pediatric cancer centers and their role in the treatment of children and adolescents with cancer.[2] At these centers, clinical trials are available for most types of cancer that occur in children and adolescents, and the opportunity to participate is offered to most patients and their families. Clinical trials for children and adolescents diagnosed with cancer are generally designed to compare potentially better therapy with current standard therapy. Other types of clinical trials test novel therapies when there is no standard therapy for a cancer diagnosis. Most of the progress in identifying curative therapies for childhood cancers has been achieved through clinical trials. Information about ongoing clinical trials is available from the NCI website.
Dramatic improvements in survival have been achieved for children and adolescents with cancer. Between 1975 and 2020, childhood cancer mortality decreased by more than 50%.[3–5] Childhood and adolescent cancer survivors require close monitoring because side effects of cancer therapy may persist or develop months or years after treatment. For information about the incidence, type, and monitoring of late effects in childhood and adolescent cancer survivors, see Late Effects of Treatment for Childhood Cancer.
Childhood cancer is a rare disease, with about 15,000 cases diagnosed annually in the United States in individuals younger than 20 years.[6] The U.S. Rare Diseases Act of 2002 defines a rare disease as one that affects populations smaller than 200,000 people in the United States. Therefore, all pediatric cancers are considered rare.
The designation of a rare tumor is not uniform among pediatric and adult groups. In adults, rare cancers are defined as those with an annual incidence of fewer than six cases per 100,000 people. They account for up to 24% of all cancers diagnosed in the European Union and about 20% of all cancers diagnosed in the United States.[7,8] In children and adolescents, the designation of a rare tumor is not uniform among international groups, as follows:
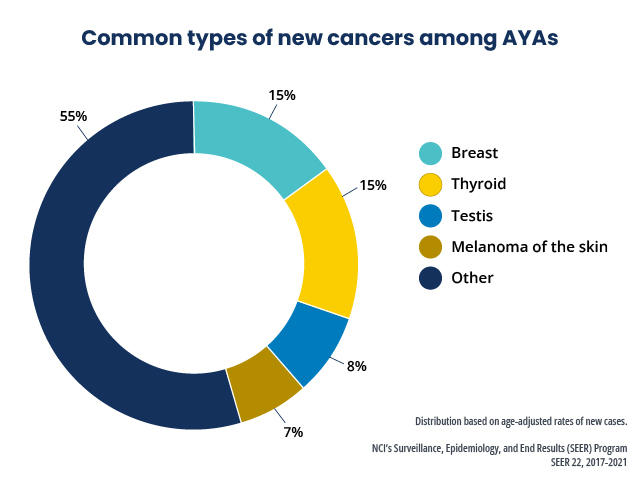
- A consensus effort between the European Union Joint Action on Rare Cancers and the European Cooperative Study Group for Rare Pediatric Cancers estimated that 11% of all cancers in patients younger than 20 years could be categorized as very rare. This consensus group defined very rare cancers as those with annual incidences of fewer than two cases per 1 million people. However, three additional histologies (thyroid carcinoma, melanoma, and testicular cancer) with incidences of more than two cases per 1 million people were also included in the very rare group due to a lack of knowledge and expertise in the management of these tumors.[9]
- The Children’s Oncology Group defines rare pediatric cancers as those listed in the International Classification of Childhood Cancer subgroup XI, which includes thyroid cancers, melanomas and nonmelanoma skin cancers, and multiple types of carcinomas (e.g., adrenocortical carcinomas, nasopharyngeal carcinomas, and most adult-type carcinomas such as breast cancers and colorectal cancers).[10] These diagnoses account for about 5% of the cancers diagnosed in children aged 0 to 14 years and about 27% of the cancers diagnosed in adolescents aged 15 to 19 years.[4]
Most cancers in subgroup XI are either melanomas or thyroid cancers, with other cancer types accounting for only 2% of the cancers diagnosed in children aged 0 to 14 years and 9.3% of the cancers diagnosed in adolescents aged 15 to 19 years.
These rare cancers are extremely challenging to study because of the relatively few patients with any individual diagnosis, the predominance of rare cancers in the adolescent population, and the small number of clinical trials for adolescents with rare cancers.
Information about these tumors may also be found in sources relevant to adults with cancer, such as Nasopharyngeal Carcinoma Treatment.
References
- Smith MA, Seibel NL, Altekruse SF, et al.: Outcomes for children and adolescents with cancer: challenges for the twenty-first century. J Clin Oncol 28 (15): 2625-34, 2010. [PUBMED Abstract]
- American Academy of Pediatrics: Standards for pediatric cancer centers. Pediatrics 134 (2): 410-4, 2014. Also available online. Last accessed February 25, 2025.
- Smith MA, Altekruse SF, Adamson PC, et al.: Declining childhood and adolescent cancer mortality. Cancer 120 (16): 2497-506, 2014. [PUBMED Abstract]
- National Cancer Institute: NCCR*Explorer: An interactive website for NCCR cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed February 25, 2025.
- Surveillance Research Program, National Cancer Institute: SEER*Explorer: An interactive website for SEER cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed December 30, 2024.
- Ward E, DeSantis C, Robbins A, et al.: Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 64 (2): 83-103, 2014 Mar-Apr. [PUBMED Abstract]
- Gatta G, Capocaccia R, Botta L, et al.: Burden and centralised treatment in Europe of rare tumours: results of RARECAREnet-a population-based study. Lancet Oncol 18 (8): 1022-1039, 2017. [PUBMED Abstract]
- DeSantis CE, Kramer JL, Jemal A: The burden of rare cancers in the United States. CA Cancer J Clin 67 (4): 261-272, 2017. [PUBMED Abstract]
- Ferrari A, Brecht IB, Gatta G, et al.: Defining and listing very rare cancers of paediatric age: consensus of the Joint Action on Rare Cancers in cooperation with the European Cooperative Study Group for Pediatric Rare Tumors. Eur J Cancer 110: 120-126, 2019. [PUBMED Abstract]
- Pappo AS, Krailo M, Chen Z, et al.: Infrequent tumor initiative of the Children’s Oncology Group: initial lessons learned and their impact on future plans. J Clin Oncol 28 (33): 5011-6, 2010. [PUBMED Abstract]
Treatment of Newly Diagnosed Childhood Nasopharyngeal Carcinoma
The European Cooperative Study Group for Pediatric Rare Tumors within the PARTNER project (Paediatric Rare Tumours Network–European Registry) have published comprehensive recommendations for the diagnosis and treatment of nasopharyngeal carcinoma in children and adolescents.[1]
Treatment options for newly diagnosed nasopharyngeal carcinoma include the following:
Combined-Modality Therapy With Chemotherapy and Radiation Therapy
High-dose radiation therapy alone has a role in managing nasopharyngeal carcinoma. However, studies (in both children and adults) show that combined-modality therapy with chemotherapy and radiation is the most effective way to treat nasopharyngeal carcinoma.[2]
Multiple studies have investigated the role of chemotherapy in the treatment of adult patients with nasopharyngeal carcinoma. The use of concomitant chemoradiation therapy has been consistently associated with a significant survival benefit, including improved locoregional disease control and reduction in distant metastases.[2] The addition of neoadjuvant or adjuvant chemotherapy to concomitant chemoradiation has further improved outcomes. The Meta-Analysis of Chemotherapy in Nasopharyngeal Carcinoma (MAC-NPC) collaborative group presented an analysis of 26 trials that included 7,080 patients. The results showed that the addition of chemotherapy to radiation therapy reduced the risk of death, and that the hazard ratio (HR) for risk of death was lowest for adjuvant or neoadjuvant chemotherapy combined with concurrent chemoradiation therapy, compared with concurrent chemoradiation therapy alone.[3]
In adult patients, recent studies investigated the use of neoadjuvant gemcitabine and cisplatin. A phase III study compared concurrent chemoradiation therapy with or without induction therapy using gemcitabine plus cisplatin for patients with locally advanced nasopharyngeal carcinoma. The study found a significant improvement in overall survival (OS) for patients who received induction chemotherapy with gemcitabine plus cisplatin, compared with those who did not receive induction chemotherapy (5-year OS rates, 87.9% vs. 78.8%; HR, 0.51; 95% confidence interval, 0.34–0.78; P = .001).[4,5]
In children, most studies have used neoadjuvant chemotherapy with cisplatin and fluorouracil (5-FU) followed by concomitant chemoradiation with single-agent cisplatin.[6–8][Level of evidence B4]; [9] Using this approach, 5-year OS rate estimates are consistently above 80%.[7–9] The following two modifications of this approach have been investigated:
- The German Society of Pediatric Oncology and Hematology (GPOH) NPC-2003 study included a 6-month maintenance therapy phase with interferon-beta. The study reported a 30-month OS rate estimate of 97.1%.[7]
- A randomized prospective trial compared cisplatin and 5-FU with and without docetaxel.[8][Level of evidence A1] The addition of docetaxel was not associated with improved outcomes.
For adults with nasopharyngeal carcinoma, gemcitabine plus cisplatin has been shown to be more effective than 5-FU plus cisplatin, both in front-line and recurrent settings.[10,11]
While nasopharyngeal carcinoma is a very chemosensitive neoplasm, high radiation doses to the nasopharynx and neck (approximately 65–70 Gy) are required for optimal locoregional control.[12–14] However, in children, studies using neoadjuvant chemotherapy have shown that it is possible to reduce the radiation dose to 55 Gy or 60 Gy for good-responding patients.[6,7,15] The GPOH reviewed 45 patients enrolled in the NPC-2003 study and an additional 21 patients who were subsequently treated per the NPC-2003 trial.[16] The 66 patients with locoregionally advanced nasopharyngeal carcinoma had an event-free survival (EFS) rate of 93.6% and an OS rate of 96.7% after a median follow-up of 73 months. Seven patients who had complete responses after induction therapy received a reduced radiation dose of 54 Gy. None of these patients experienced a relapse. In young patients with advanced locoregional nasopharyngeal carcinoma, excellent long-term survival rates can be achieved using multimodal treatment, including interferon-beta. Radiation doses may be reduced in patients with complete remission after induction chemotherapy. Reduced radiation doses may limit late effects related to radiation exposure.
The Children’s Oncology Group performed a prospective trial to evaluate the impact of induction chemotherapy and concurrent chemoradiation therapy.[9] Patients were scheduled to receive three cycles of induction chemotherapy with cisplatin and 5-FU, followed by chemoradiation therapy with three cycles of cisplatin. Patients with complete or partial responses to induction chemotherapy received 61.2 Gy of radiation to the nasopharynx and neck, and patients with stable disease received 71.2 Gy of radiation. After a feasibility analysis, the study was amended to reduce cisplatin to two cycles during chemoradiation therapy. Results of the study include the following:
- The 5-year EFS rate estimate was 84.3%, and the OS rate estimate was 89.2%.
- The 5-year EFS rates were 100% for patients with stage IIb disease, 82.8% for patients with stage III disease, and 82.7% for patients with stage IV disease.
- The 5-year cumulative incidence estimates of local, distant, and combined relapses were 3.7%, 8.7%, and 1.8%, respectively.
- Patients who were treated with three chemoradiation therapy cycles of cisplatin were observed to have higher 5-year postinduction EFS rates than patients who were treated with two cycles, although the difference was not statistically significant (90.7% vs. 81.2%; P = .14).
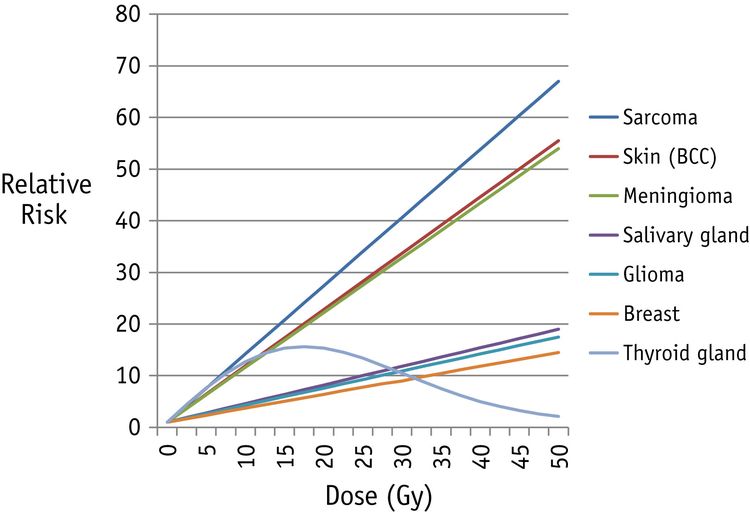
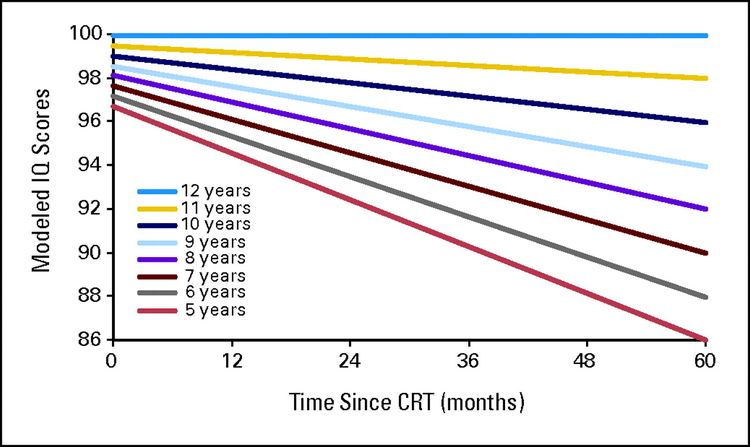
The combination of cisplatin-based chemotherapy and high doses of radiation therapy to the nasopharynx and neck are associated with a high probability of hearing loss, hypothyroidism and panhypopituitarism, trismus, xerostomia, dental problems, and chronic sinusitis or otitis.[6,17,18]; [19][Level of evidence C1] The use of proton radiation therapy may reduce the toxicity to the brain and skull base region without compromising disease control.[20] For more information, see Late Effects of Treatment for Childhood Cancer.
In a group of 549 pediatric patients with nasopharyngeal carcinoma diagnosed between 2005 and 2021, recursive partitioning (i.e., successive grouping) was performed based on stage and Epstein-Barr virus (EBV) viral load. This resulted in three groups of patients: low-risk patients, intermediate-risk patients, and high-risk patients.[21]
- Intermediate-risk patients (stage IVa nasopharyngeal carcinoma and <4,000 copies/mL of EBV) had significant responses with induction chemotherapy followed by concurrent chemotherapy and radiation therapy. Their progression-free survival (PFS) and distant metastases‒free survival rates were significantly improved, compared with those who received only concurrent chemotherapy and radiation therapy.
- In contrast, there were no significant differences between these two treatment regimens in low-risk and high-risk patients.
Surgery
Surgery has a limited role in the management of nasopharyngeal carcinoma. The disease is usually considered unresectable because of extensive local spread.
Immunotherapy With Checkpoint Inhibitors
The U.S. Food and Drug Administration (FDA) approved the anti-PD-1 monoclonal antibody toripalimab-tpzi in combination with cisplatin and gemcitabine for first-line treatment of adults with metastatic or recurrent, locally advanced nasopharyngeal carcinoma. The approval was based on the results of a phase III placebo-controlled clinical trial. Patients received toripalimab-tpzi or placebo in combination with gemcitabine plus cisplatin every 3 weeks for up to six cycles, followed by monotherapy with toripalimab-tpzi or placebo. Patients randomly assigned to receive toripalimab-tpzi had superior PFS and OS rates. The 1-year and 2-year PFS rates were 59.0% versus 32.9% and 44.8% versus 25.4% in the toripalimab-tpzi and placebo groups, respectively. Corresponding OS rates at 2 years were 78.0% versus 65.1%, respectively. At 3 years, the OS rates were 64.5% versus 49.2%, respectively.[22][Level of evidence B1]
Treatment Options Under Clinical Evaluation for Newly Diagnosed Childhood Nasopharyngeal Carcinoma
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, see the ClinicalTrials.gov website.
The following is an example of a national and/or institutional clinical trial that is currently being conducted:
- ARAR2221 (NCT06064097) (A Study Using Nivolumab, in Combination with Chemotherapy Drugs to Treat Nasopharyngeal Carcinoma): This study will evaluate the safety of combining induction chemotherapy with an anti-PD-1 immune checkpoint inhibitor (nivolumab) in children, adolescents, and young adults with nasopharyngeal carcinoma. It will also estimate the 2-year EFS rate of patients treated with induction chemoimmunotherapy using gemcitabine and cisplatin, followed by consolidation chemotherapy, radiation therapy, immunotherapy (cisplatin, nivolumab, and response-adjusted, dose de-escalated radiation therapy), and nivolumab maintenance therapy.
The treatment plan in the ARAR2221 trial was modeled after therapy that was effective in phase III trials for adults with nasopharyngeal carcinoma.
References
- Ben-Ami T, Kontny U, Surun A, et al.: Nasopharyngeal carcinoma in children and adolescents: The EXPeRT/PARTNER diagnostic and therapeutic recommendations. Pediatr Blood Cancer 68 (Suppl 4): e29018, 2021. [PUBMED Abstract]
- Chen YP, Chan ATC, Le QT, et al.: Nasopharyngeal carcinoma. Lancet 394 (10192): 64-80, 2019. [PUBMED Abstract]
- Blanchard P, Lee AWM, Carmel A, et al.: Meta-analysis of chemotherapy in nasopharynx carcinoma (MAC-NPC): An update on 26 trials and 7080 patients. Clin Transl Radiat Oncol 32: 59-68, 2022. [PUBMED Abstract]
- Zhang Y, Chen L, Hu GQ, et al.: Gemcitabine and Cisplatin Induction Chemotherapy in Nasopharyngeal Carcinoma. N Engl J Med 381 (12): 1124-1135, 2019. [PUBMED Abstract]
- Zhang Y, Chen L, Hu GQ, et al.: Final Overall Survival Analysis of Gemcitabine and Cisplatin Induction Chemotherapy in Nasopharyngeal Carcinoma: A Multicenter, Randomized Phase III Trial. J Clin Oncol 40 (22): 2420-2425, 2022. [PUBMED Abstract]
- Casanova M, Bisogno G, Gandola L, et al.: A prospective protocol for nasopharyngeal carcinoma in children and adolescents: the Italian Rare Tumors in Pediatric Age (TREP) project. Cancer 118 (10): 2718-25, 2012. [PUBMED Abstract]
- Buehrlen M, Zwaan CM, Granzen B, et al.: Multimodal treatment, including interferon beta, of nasopharyngeal carcinoma in children and young adults: preliminary results from the prospective, multicenter study NPC-2003-GPOH/DCOG. Cancer 118 (19): 4892-900, 2012. [PUBMED Abstract]
- Casanova M, Özyar E, Patte C, et al.: International randomized phase 2 study on the addition of docetaxel to the combination of cisplatin and 5-fluorouracil in the induction treatment for nasopharyngeal carcinoma in children and adolescents. Cancer Chemother Pharmacol 77 (2): 289-98, 2016. [PUBMED Abstract]
- Rodriguez-Galindo C, Krailo MD, Krasin MJ, et al.: Treatment of Childhood Nasopharyngeal Carcinoma With Induction Chemotherapy and Concurrent Chemoradiotherapy: Results of the Children’s Oncology Group ARAR0331 Study. J Clin Oncol 37 (35): 3369-3376, 2019. [PUBMED Abstract]
- Zhang L, Huang Y, Hong S, et al.: Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet 388 (10054): 1883-1892, 2016. [PUBMED Abstract]
- Liu LT, Liu H, Huang Y, et al.: Concurrent chemoradiotherapy followed by adjuvant cisplatin-gemcitabine versus cisplatin-fluorouracil chemotherapy for N2-3 nasopharyngeal carcinoma: a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Oncol 24 (7): 798-810, 2023. [PUBMED Abstract]
- Langendijk JA, Leemans ChR, Buter J, et al.: The additional value of chemotherapy to radiotherapy in locally advanced nasopharyngeal carcinoma: a meta-analysis of the published literature. J Clin Oncol 22 (22): 4604-12, 2004. [PUBMED Abstract]
- Yan M, Kumachev A, Siu LL, et al.: Chemoradiotherapy regimens for locoregionally advanced nasopharyngeal carcinoma: A Bayesian network meta-analysis. Eur J Cancer 51 (12): 1570-9, 2015. [PUBMED Abstract]
- Ribassin-Majed L, Marguet S, Lee AWM, et al.: What Is the Best Treatment of Locally Advanced Nasopharyngeal Carcinoma? An Individual Patient Data Network Meta-Analysis. J Clin Oncol 35 (5): 498-505, 2017. [PUBMED Abstract]
- Yao JJ, Jin YN, Lin YJ, et al.: The feasibility of reduced-dose radiotherapy in childhood nasopharyngeal carcinoma with favorable response to neoadjuvant chemotherapy. Radiother Oncol 178: 109414, 2023. [PUBMED Abstract]
- Römer T, Franzen S, Kravets H, et al.: Multimodal Treatment of Nasopharyngeal Carcinoma in Children, Adolescents and Young Adults-Extended Follow-Up of the NPC-2003-GPOH Study Cohort and Patients of the Interim Cohort. Cancers (Basel) 14 (5): , 2022. [PUBMED Abstract]
- Cheuk DK, Billups CA, Martin MG, et al.: Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117 (1): 197-206, 2011. [PUBMED Abstract]
- Sahai P, Mohanti BK, Sharma A, et al.: Clinical outcome and morbidity in pediatric patients with nasopharyngeal cancer treated with chemoradiotherapy. Pediatr Blood Cancer 64 (2): 259-266, 2017. [PUBMED Abstract]
- Hu S, Xu X, Xu J, et al.: Prognostic factors and long-term outcomes of nasopharyngeal carcinoma in children and adolescents. Pediatr Blood Cancer 60 (7): 1122-7, 2013. [PUBMED Abstract]
- Uezono H, Indelicato DJ, Rotondo RL, et al.: Proton therapy following induction chemotherapy for pediatric and adolescent nasopharyngeal carcinoma. Pediatr Blood Cancer 66 (12): e27990, 2019. [PUBMED Abstract]
- Liang YJ, Wen DX, Luo MJ, et al.: Induction or adjuvant chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in paediatric nasopharyngeal carcinoma in the IMRT era: A recursive partitioning risk stratification analysis based on EBV DNA. Eur J Cancer 159: 133-143, 2021. [PUBMED Abstract]
- Mai HQ, Chen QY, Chen D, et al.: Toripalimab or placebo plus chemotherapy as first-line treatment in advanced nasopharyngeal carcinoma: a multicenter randomized phase 3 trial. Nat Med 27 (9): 1536-1543, 2021. [PUBMED Abstract]
Treatment of Relapsed or Refractory Childhood Nasopharyngeal Carcinoma
The outcome is poor for patients with relapsed or refractory nasopharyngeal carcinoma, and most patients present with distant metastases.
Treatment options for relapsed or refractory nasopharyngeal carcinoma include the following:
Chemotherapy
Long-term remissions can be achieved with conventional chemotherapy. In a retrospective review of 14 pediatric patients with relapsed nasopharyngeal carcinoma who were treated with varying chemotherapy regimens, the 3-year event-free survival rate was 34%, and the overall survival rate was 44%.[1]
Immunotherapy
Given the unique pathogenesis of nasopharyngeal carcinoma, immunotherapy has been explored for patients with refractory disease, as follows:
- The use of Epstein-Barr virus (EBV)–specific cytotoxic T-lymphocyte therapy is a promising approach, with minimal toxicity and evidence of significant antitumor activity in patients with relapsed or refractory nasopharyngeal carcinoma.[2] In a phase I/II study of EBV-specific cytotoxic T-lymphocyte therapy in patients with refractory disease, response rates were observed in 33.3% of patients. Long-term remissions were obtained in 62% of patients treated in their second or subsequent remission.[3]
- Anti–programmed death 1 (PD-1) and programmed death-ligand 1 (PD-L1) monoclonal antibodies have been studied in adults with refractory nasopharyngeal carcinoma. In a meta-analysis that included nine studies and 842 patients with recurrent or metastatic nasopharyngeal carcinoma who received PD-1 inhibitors, the objective response rate was 24% (95% confidence interval [CI], 21%–26%), the 1-year progression-free survival rate was 25% (95% CI, 18%–32%), and the 1-year overall survival rate was 53% (95% CI, 37%–68%).[4]
Treatment Options Under Clinical Evaluation for Relapsed or Refractory Childhood Nasopharyngeal Carcinoma
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, see the ClinicalTrials.gov website.
References
- DeRenzo C, Lam C, Rodriguez-Galindo C, et al.: Salvage regimens for pediatric patients with relapsed nasopharyngeal carcinoma. Pediatr Blood Cancer 66 (1): e27469, 2019. [PUBMED Abstract]
- Straathof KC, Bollard CM, Popat U, et al.: Treatment of nasopharyngeal carcinoma with Epstein-Barr virus–specific T lymphocytes. Blood 105 (5): 1898-904, 2005. [PUBMED Abstract]
- Louis CU, Straathof K, Bollard CM, et al.: Adoptive transfer of EBV-specific T cells results in sustained clinical responses in patients with locoregional nasopharyngeal carcinoma. J Immunother 33 (9): 983-90, 2010 Nov-Dec. [PUBMED Abstract]
- Luo J, Xiao W, Hua F, et al.: Efficacy and safety of PD-1 inhibitors in recurrent or metastatic nasopharyngeal carcinoma patients after failure of platinum-containing regimens: a systematic review and meta-analysis. BMC Cancer 23 (1): 1172, 2023. [PUBMED Abstract]
Latest Updates to This Summary (08/23/2024)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
This summary was comprehensively reviewed.
This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood nasopharyngeal cancer. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Childhood Nasopharyngeal Cancer Treatment are:
- Denise Adams, MD (Children’s Hospital Boston)
- Karen J. Marcus, MD, FACR (Dana-Farber of Boston Children’s Cancer Center and Blood Disorders Harvard Medical School)
- William H. Meyer, MD
- Paul A. Meyers, MD (Memorial Sloan-Kettering Cancer Center)
- Thomas A. Olson, MD (Aflac Cancer and Blood Disorders Center of Children’s Healthcare of Atlanta – Egleston Campus)
- Alberto S. Pappo, MD (St. Jude Children’s Research Hospital)
- Arthur Kim Ritchey, MD (Children’s Hospital of Pittsburgh of UPMC)
- Carlos Rodriguez-Galindo, MD (St. Jude Children’s Research Hospital)
- Stephen J. Shochat, MD (St. Jude Children’s Research Hospital)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website’s Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Nasopharyngeal Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: /types/head-and-neck/hp/child/nasopharyngeal-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 29320137]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
Based on the strength of the available evidence, treatment options may be described as either “standard” or “under clinical evaluation.” These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.