Pituitary Tumors Treatment (PDQ®)–Health Professional Version
General Information About Pituitary Tumors
Pituitary tumors account for 10% to 25% of all intracranial neoplasms. Depending on the study cited, pituitary tumors can be classified into one of the following three groups according to their biological behavior:[1,2]
- Benign adenoma.
- Invasive adenoma.
- Carcinoma.
Adenomas account for the largest portion of pituitary neoplasms with an overall estimated prevalence of 17%. Few adenomas are symptomatic.[3] In addition, pituitary adenomas may be distinguished anatomically as intrapituitary, intrasellar, diffuse, and invasive.[4] Approximately 35% of pituitary adenomas are invasive, and may invade the dura mater, cranial bone, or sphenoid sinus.[5] Carcinomas account for 0.1% to 0.2% of all pituitary tumors.[6,7]
Clinical Presentation
The most characteristic presenting features of pituitary adenomas include inappropriate pituitary hormone secretion and visual field deficits.[8]
Rare signs and symptoms of pituitary disease include:[8]
- Cranial nerve palsies.
- Temporal lobe epilepsy.
- Hydrocephalus.
- Cerebrospinal fluid rhinorrhea.
The signs and symptoms commonly associated with pituitary tumors are derived from each specific cell type (i.e., prolactinomas, corticotroph adenomas, somatotroph adenomas, thyrotroph adenomas, and nonfunctioning adenomas).
Prolactin-producing pituitary tumors
Signs and symptoms of prolactin-producing pituitary tumors, also known as prolactinomas and lactotroph adenomas, may include:[8]
- Headache.
- Visual field deficits.
- Oligomenorrhea or amenorrhea.
- Reduced fertility.
- Loss of libido.
- Erectile dysfunction.
- Galactorrhea in the estrogen-primed female breast.
Adrenocorticotrophic hormone–producing pituitary tumors
Signs and symptoms of adrenocorticotrophic hormone–producing pituitary tumors, also known as corticotroph adenomas, may include:[8]
- Headache.
- Visual field deficits.
- Proximal myopathy.
- Centripetal fat distribution.
- Neuropsychiatric symptoms.
- Striae.
- Easy bruising.
- Skin thinning.
- Hirsutism.
- Osteopenia.
Growth hormone–producing pituitary tumors
Signs and symptoms of growth hormone–producing pituitary tumors, also known as somatotroph adenomas, may include:[8]
- Headache.
- Visual field deficits.
- Growth of hands and feet.
- Coarsening of facial features.
- Carpal tunnel syndrome.
- Snoring and obstructive sleep apnea.
- Jaw growth and prognathism.
- Osteoarthritis and arthralgia.
- Excessive sweating.
- Dysmorphophobia.
Thyrotropin-producing pituitary tumors
Signs and symptoms of thyrotropin (thyroid-stimulating hormone)-producing tumors, also known as thyrotroph adenomas, may include:[9]
- Heart palpitations.
- Tremor.
- Weight loss.
- Insomnia.
- Hyperdefecation.
- Sweating.
Nonfunctioning adenomas
Signs and symptoms of nonfunctioning adenomas (most commonly gonadotroph adenomas) may include:[10]
- Headache.
- Visual field deficits.
- Pituitary insufficiency, which is due to compression of the pituitary stalk or destruction of normal pituitary tissue by the tumor. It predominantly manifests as secondary hypogonadism.
- Rarely, ovarian overstimulation, testicular enlargement, or increased testosterone levels.
In addition to cell-type specific presentations, pituitary apoplexy (i.e., pituitary adenoma apoplexy) represents another important clinical presentation of pituitary adenomas. Pituitary apoplexy can result from an acute hemorrhagic or ischemic infarction of the pituitary in patients harboring often unrecognized secreting or nonfunctioning pituitary adenomas. In a series analyzing 40 cases of pituitary apoplexy, the presenting signs and symptoms included headache (63%), vomiting (50%), visual field defects (61%), ocular paresis (40%), mental deterioration (13%), hyponatremia (13%), and syncope (5%). There were only four cases in which the pituitary tumor was diagnosed before the apoplexy presentation.[11]
The development of pituitary adenomas may also occur as a component of one of the following familial cancer syndromes:[8]
- Multiple endocrine neoplasia type 1.
- Carney complex (e.g., cardiac myxomas, spotty skin pigmentation, and tumors of the adrenal gland and anterior pituitary).
- Isolated familial acromegaly.
Other lesions should be considered in the differential diagnosis of sellar masses. Although rare, lymphocytic (i.e., autoimmune) hypophysitis should be considered in the differential diagnosis of any nonsecreting pituitary mass, especially when occurring during pregnancy or postpartum.[12] In addition, the clinician should consider craniopharyngioma and Rathke cleft cyst in the differential diagnosis of pituitary tumors. Sellar masses may also result from tumors that are metastatic to the pituitary. This typically occurs as a part of a generalized metastatic spread and is usually associated with five or more additional metastatic sites, especially osseous; breast and lung cancer are the most common primary neoplasms metastasizing to the pituitary.[13]
References
- Asa SL, Ezzat S: The cytogenesis and pathogenesis of pituitary adenomas. Endocr Rev 19 (6): 798-827, 1998. [PUBMED Abstract]
- Landman RE, Horwith M, Peterson RE, et al.: Long-term survival with ACTH-secreting carcinoma of the pituitary: a case report and review of the literature. J Clin Endocrinol Metab 87 (7): 3084-9, 2002. [PUBMED Abstract]
- Ezzat S, Asa SL, Couldwell WT, et al.: The prevalence of pituitary adenomas: a systematic review. Cancer 101 (3): 613-9, 2004. [PUBMED Abstract]
- Kovacs K, Horvath E, Vidal S: Classification of pituitary adenomas. J Neurooncol 54 (2): 121-7, 2001. [PUBMED Abstract]
- Scheithauer BW, Kovacs KT, Laws ER, et al.: Pathology of invasive pituitary tumors with special reference to functional classification. J Neurosurg 65 (6): 733-44, 1986. [PUBMED Abstract]
- Pernicone PJ, Scheithauer BW, Sebo TJ, et al.: Pituitary carcinoma: a clinicopathologic study of 15 cases. Cancer 79 (4): 804-12, 1997. [PUBMED Abstract]
- Ragel BT, Couldwell WT: Pituitary carcinoma: a review of the literature. Neurosurg Focus 16 (4): E7, 2004. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
- Vance ML: Treatment of patients with a pituitary adenoma: one clinician’s experience. Neurosurg Focus 16 (4): E1, 2004. [PUBMED Abstract]
- Losa M, Mortini P, Barzaghi R, et al.: Endocrine inactive and gonadotroph adenomas: diagnosis and management. J Neurooncol 54 (2): 167-77, 2001. [PUBMED Abstract]
- Lubina A, Olchovsky D, Berezin M, et al.: Management of pituitary apoplexy: clinical experience with 40 patients. Acta Neurochir (Wien) 147 (2): 151-7; discussion 157, 2005. [PUBMED Abstract]
- Caturegli P, Newschaffer C, Olivi A, et al.: Autoimmune hypophysitis. Endocr Rev 26 (5): 599-614, 2005. [PUBMED Abstract]
- Komninos J, Vlassopoulou V, Protopapa D, et al.: Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab 89 (2): 574-80, 2004. [PUBMED Abstract]
Cellular Classification of Pituitary Tumors
Pituitary adenomas can be classified according to staining affinities of the cell cytoplasm, size, endocrine activity, histological characteristics, hormone production and contents, ultrastructural features, granularity of the cell cytoplasm, cellular composition, cytogenesis, and growth pattern.[1] Recent classifications, however, omit criteria based on tinctorial stains (i.e., acidophilic, basophilic, and chromophobic) because of the poor correlation between staining affinities of the cell cytoplasm and other pathological features of pituitary tumors, such as the type of hormone produced and cellular derivation.[1,2]
A unifying pituitary adenoma classification incorporates the histological, immunocytochemical, and electron microscopic studies of the tumor cells. It also stresses the importance of hormone production, cellular composition, and cytogenesis. This classification emphasizes the structure-function relationship and attempts to correlate morphologic features with secretory activity.[1]
Pituitary adenomas may be classified based on the following:[2]
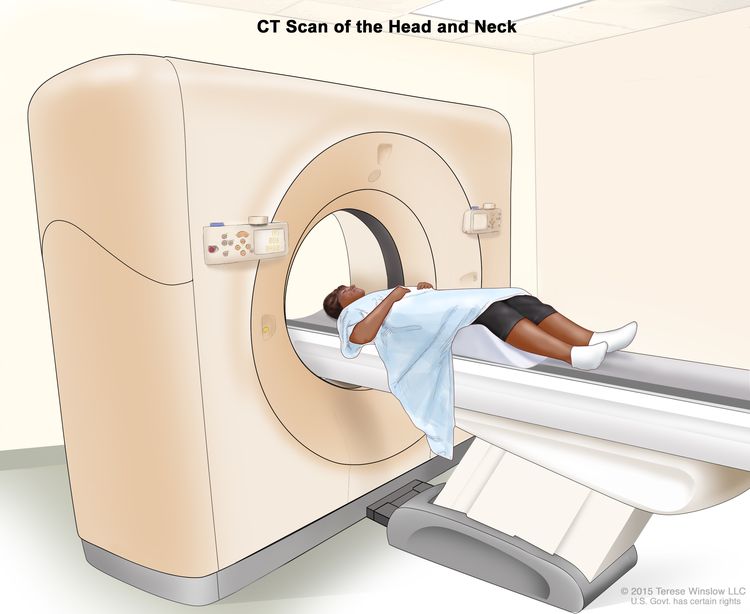
- An anatomical approach, which classifies pituitary tumors by size based on radiological findings. Tumors are divided into microadenomas (i.e., greatest diameter <10 mm) and macroadenomas (i.e., greatest diameter ≥10 mm).[3] Most pituitary adenomas are microadenomas. Historically, the most widely used radioanatomical classification was based primarily on a neuroradiological examination including skull x-rays, pneumoencephalography, polytomography, and carotid angiography [4] and subsequently validated by more accurate computed tomography (CT) and magnetic resonance imaging (MRI). This radioanatomical classification places adenomas into one of five grades (0–IV).[5] For more information, see the Stage Information For Pituitary Tumors section.
MRI is the imaging modality of choice for the diagnosis of pituitary disorders because of its multiplanar capability and good soft tissue contrast enhancement.[3] Sagittal T1-weighted images, clearly displaying the anterior and posterior lobes and the stalk on the same plane, and coronal images, displaying the relation between the pituitary and cavernous sinuses, are optimal for identifying a pituitary adenoma. A 3-mm thin slice typically is used to obtain optimal resolution.[6] CT may also be a useful diagnostic tool with coronal scans providing the optimal view;[7] however, CT may be less sensitive than MRI in this application.[8] For each imaging technique, a focal hypointensity within the pituitary gland is considered abnormal and suggestive of an adenoma. MRI is also the best diagnostic imaging choice for pituitary carcinomas; metastases may be found in the cerebral lobes, cerebellum, spinal cord, leptomeninges, and subarachnoid space.[9]
- Histological criteria, which use the following:
- Immunohistological characterization of the tumors in terms of hormone production. Immunocytochemical staining for pituitary hormones generally correlates with hormone serum levels. Twenty percent of pituitary adenomas have no identifiable hormone production.
- Ultrastructural criteria, which can confirm that nonfunctional lesions are of pituitary origin and characterize the cytological differentiation of tumor cells in terms of anterior pituitary cell types.
- Functional criteria, which are used to define tumors in terms of their endocrine activity. Clinical endocrinologists often use the functional classification of pituitary adenomas and define these tumors based on their hormonal activity in vivo. A retrospective review of the pituitary adenoma literature indicates that prolactinomas are the most common form of pituitary adenoma as determined by immunohistochemical criteria; tumors secreting adrenocorticotropic hormone (ACTH), growth hormone (GH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH) follow in decreasing frequency.[3,10] However, functionally inactive pituitary adenomas make up approximately 30% to 35% of the pituitary tumors in most series and are the most common type of macroadenoma.[11]
Using functional criteria, pituitary adenomas can be characterized as follows:[5]
- Prolactin (PRL)-producing, also known as lactotroph, adenomas causing hyperprolactinemia and its clinical sequelae.
- ACTH-producing, also known as corticotroph, adenomas associated with Cushing or Nelson syndromes.
- GH-producing, also known as somatotroph, adenomas associated with acromegaly and/or gigantism.
- Rare thyrotropin TSH-producing, also known as thyrotroph, tumors.
- The large group of clinically nonfunctioning (i.e., the endocrine-inactive) adenomas. This group is predominantly composed of gonadotroph adenomas. Gonadotroph adenomas synthesize follicle-stimulating hormone (FSH) and/or LH, or the alpha or beta subunits of these heterodimers. They are usually detected incidentally or because of the presence of neurological symptoms. Gonadotroph adenomas are inefficient secretors of the hormones they produce, so they rarely result in a clinically recognizable hormonal hypersecretion syndrome.
- Because of the relative abundance of adenomas that secrete both GH and PRL, the category of mixed adenomas has also become a designation.
Hormone-secreting pituitary carcinomas may elicit similar signs and symptoms according to the particular hormone that is secreted. They may also produce signs and symptoms related to malignant spread.[9] Because no unequivocal histopathological features of carcinoma exist, the diagnosis of malignancy is reserved for pituitary neoplasms that have metastasized to remote areas of the central nervous system (CNS) or outside of the CNS.[12–14] In a review of 95 cases of pituitary carcinoma, 68% of the cases were hormone-producing, and PRL (26%) and ACTH (25%) were the most common hormonal subtypes.[15] Pituitary carcinomas producing GH were the second most common of the hormonal subtypes, and FSH/LH-producing and TSH-producing carcinomas were even more rarely reported. Other reports indicate that as many as 88% of pituitary carcinomas are endocrinologically active, and ACTH-secreting tumors are the most common.[9] Although only 2% to 10% of pituitary adenomas are ACTH-secreting, the percentage of pituitary carcinomas that secrete ACTH is estimated to be much higher at 25% to 34%.[15–19] In a series of 15 cases, carcinomas showed a greater tendency toward systemic metastasis than craniospinal metastasis; the rate of systemic metastasis was 71% for PRL-producing cell tumors and 57% for ACTH-producing tumors.[16]
Prolactin (PRL)-Producing Pituitary Tumors
PRL-producing pituitary tumors, also known as prolactinomas and lactotroph adenomas, secrete PRL and are typically an intrasellar tumor. In women, these adenomas are often small (<10 mm). However, in either sex they can become large enough to enlarge the sella turcica. These adenomas represent the most common hormone-producing pituitary tumors and account for 25% to 41% of tumor specimens.[3]
Adrenocorticotrophic Hormone (ACTH)–Producing Pituitary Tumors
The major manifestation of ACTH-producing pituitary tumors, also known as corticotroph adenomas, is secretion of ACTH, which results in Cushing syndrome. These tumors are initially confined to the sella turcica, but they may enlarge and become invasive after bilateral adrenalectomy (i.e., Nelson syndrome). These adenomas represent the second or third most common hormone-producing pituitary tumors, depending on the series; in one series, these tumors accounted for 10% of all tumor specimens.[1,3]
Growth Hormone (GH)–Producing Pituitary Tumors
GH-producing pituitary tumors, also known as somatotroph adenomas, produce GH, resulting in gigantism in younger patients and acromegaly in others. Suprasellar extension is not uncommon. These adenomas represent the second or third most common hormone-producing pituitary tumors, depending on the series; in one series, these adenomas accounted for 13% of tumor specimens.[1,3]
Thyrotropin-Producing Pituitary Tumors
Thyrotroph-producing pituitary tumors, also known as thyrotroph adenomas, secrete TSH, also known as thyrotropin, which results in hyperthyroidism without TSH suppression. Many are large and invasive, may be plurihormonal, and secrete both GH and/or PRL.[20] These tumors are rare and account for no more than 2% of tumor specimens.[1,3,20]
Gonadotroph (FSH-Producing and/or LH-Producing) Adenomas
Gonadotroph adenomas may secrete FSH and/or LH, or the alpha or beta subunits that comprise these heterodimers. Depending on the patient’s sex, this secretion may result in ovarian overstimulation, increased testosterone levels, testicular enlargement, and pituitary insufficiency caused by compression of the pituitary stalk or destruction of normal pituitary tissue by the tumor. Many gonadotroph tumors, however, are unassociated with clinical or biochemical evidence of hormone excess and may be considered to be nonfunctioning or endocrine-inactive tumors.[21] Functional, clinically detectable gonadotroph adenomas are rare.[5]
Plurihormonal Adenomas
Plurihormonal tumors produce more than one hormone. Morphologically, they can be either monomorphous or plurimorphous. Monomorphous plurihormonal adenomas consist of one cell population that produces two or more hormones. The adenoma cells often differ from nontumorous adenohypophysial cells, and their cellular derivation may remain obscure despite extensive morphological studies. Plurimorphous plurihormonal adenomas consist of two or more distinct cell types, and each produces one hormone.[1] Thyrotroph adenomas are often plurihormonal.[20]
Nonfunctioning (Endocrine-Inactive) Adenomas
These tumors arise from the adenohypophysis and cause symptoms when they extend beyond the sella, which results in pressure on the surrounding structures rather than secretion of a hormonally active substance. Endocrine-inactive adenomas show positive immunostaining for one or more pituitary hormones;[1] however, they are not associated with clinical and biochemical evidence of hormone excess. Gonadotrophic hormones, as detected by antisera to beta-FSH and beta-LH, are present in many clinically nonfunctioning adenomas. Some of these adenomas are recognized by electron microscopy to have gonadotrophic differentiation, but some have characteristics of less well-differentiated cells and resemble the null cells that were initially thought to be undifferentiated precursors of adenohypophysial cells.[5] Endocrine-inactive pituitary adenomas account for approximately 30% to 35% of the pituitary tumors in most series and are the most common type of macroadenoma.[11]
Oncocytic Tumors
Oncocytic tumors of the pituitary, also known as pituitary oncocytomas, are characterized by an abundance of mitochondria. These mitochondria may fill up to 50% of the cytoplasmic area, which is normally around 8%, and obscure other organelles. These tumors are usually not associated with clinical and biochemical evidence of hormone excess; in some cases, they may be accompanied by various degrees of hypopituitarism and/or mild hyperprolactinemia. Oncocytic change may occur in several other pituitary tumor types.[1]
Carcinomas
Pituitary carcinomas are usually endocrinologically functional, and ACTH-producing and PRL-producing tumors are the most frequent types.[2,9] The histological and cytological characteristics of pituitary carcinomas vary from bland and monotonous to frankly malignant.[22] Carcinomas show a variable degree of nuclear atypia and cellular pleomorphism, but they also show significantly higher mitotic rates and cell proliferation indices than adenomas.[2] Carcinomas account for 0.1% to 0.2% of all pituitary tumors.[9,16]
Metastatic Tumors
Breast and lung cancers are the most common primary sites for neoplasms that have metastasized to the pituitary. Although tumors that are metastatic to the pituitary have been reported to be as high as 28% in autopsy series, most metastatic tumors are clinically silent.[23]
Other Tumors
Other tumors that arise in the pituitary include craniopharyngiomas, meningiomas, and germ cell tumors; the rare granular cell tumors, pituicytomas, and gangliogliomas; and the even rarer gangliocytomas, lymphomas, astrocytomas, and ependymomas.[2]
References
- Kovacs K, Horvath E, Vidal S: Classification of pituitary adenomas. J Neurooncol 54 (2): 121-7, 2001. [PUBMED Abstract]
- Ironside JW: Best Practice No 172: pituitary gland pathology. J Clin Pathol 56 (8): 561-8, 2003. [PUBMED Abstract]
- Ezzat S, Asa SL, Couldwell WT, et al.: The prevalence of pituitary adenomas: a systematic review. Cancer 101 (3): 613-9, 2004. [PUBMED Abstract]
- Hardy J: Transsphenoidal surgery of hypersecreting pituitary tumors. In: Kohler PO, Ross GT, eds.: Diagnosis and treatment of pituitary tumors: proceedings of a conference sponsored jointly by the National Institute of Child Health and Human Development and the National Cancer Institute, January 15-17, 1973, Bethesda, Md. Amsterdam, The Netherlands: Excerpta medica, 1973, pp 179-98.
- Asa SL, Ezzat S: The cytogenesis and pathogenesis of pituitary adenomas. Endocr Rev 19 (6): 798-827, 1998. [PUBMED Abstract]
- Elster AD: Modern imaging of the pituitary. Radiology 187 (1): 1-14, 1993. [PUBMED Abstract]
- Chambers EF, Turski PA, LaMasters D, et al.: Regions of low density in the contrast-enhanced pituitary gland: normal and pathologic processes. Radiology 144 (1): 109-13, 1982. [PUBMED Abstract]
- Hall WA, Luciano MG, Doppman JL, et al.: Pituitary magnetic resonance imaging in normal human volunteers: occult adenomas in the general population. Ann Intern Med 120 (10): 817-20, 1994. [PUBMED Abstract]
- Ragel BT, Couldwell WT: Pituitary carcinoma: a review of the literature. Neurosurg Focus 16 (4): E7, 2004. [PUBMED Abstract]
- McComb DJ, Ryan N, Horvath E, et al.: Subclinical adenomas of the human pituitary. New light on old problems. Arch Pathol Lab Med 107 (9): 488-91, 1983. [PUBMED Abstract]
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
- Scheithauer BW, Kovacs KT, Laws ER, et al.: Pathology of invasive pituitary tumors with special reference to functional classification. J Neurosurg 65 (6): 733-44, 1986. [PUBMED Abstract]
- Della Casa S, Corsello SM, Satta MA, et al.: Intracranial and spinal dissemination of an ACTH secreting pituitary neoplasia. Case report and review of the literature. Ann Endocrinol (Paris) 58 (6): 503-9, 1997. [PUBMED Abstract]
- Kemink SA, Wesseling P, Pieters GF, et al.: Progression of a Nelson’s adenoma to pituitary carcinoma; a case report and review of the literature. J Endocrinol Invest 22 (1): 70-5, 1999. [PUBMED Abstract]
- Kaltsas GA, Grossman AB: Malignant pituitary tumours. Pituitary 1 (1): 69-81, 1998. [PUBMED Abstract]
- Pernicone PJ, Scheithauer BW, Sebo TJ, et al.: Pituitary carcinoma: a clinicopathologic study of 15 cases. Cancer 79 (4): 804-12, 1997. [PUBMED Abstract]
- Kovacs K, Horvath E: Pathology of pituitary tumors. Endocrinol Metab Clin North Am 16 (3): 529-51, 1987. [PUBMED Abstract]
- Thapar K, Scheithauer BW, Kovacs K, et al.: p53 expression in pituitary adenomas and carcinomas: correlation with invasiveness and tumor growth fractions. Neurosurgery 38 (4): 765-70; discussion 770-1, 1996. [PUBMED Abstract]
- Garrão AF, Sobrinho LG, Pedro-Oliveira, et al.: ACTH-producing carcinoma of the pituitary with haematogenic metastases. Eur J Endocrinol 137 (2): 176-80, 1997. [PUBMED Abstract]
- Teramoto A, Sanno N, Tahara S, et al.: Pathological study of thyrotropin-secreting pituitary adenoma: plurihormonality and medical treatment. Acta Neuropathol (Berl) 108 (2): 147-53, 2004. [PUBMED Abstract]
- Snyder PJ: Extensive personal experience: gonadotroph adenomas. J Clin Endocrinol Metab 80 (4): 1059-61, 1995. [PUBMED Abstract]
- Pernicone PJ, Scheithauer BW: Invasive pituitary adenoma and pituitary carcinoma. In: Thapar K, Kovacs K, Scheithauer BW, et al., eds.: Diagnosis and Management of Pituitary Tumors. Humana Press, 2001, pp 369-86.
- Komninos J, Vlassopoulou V, Protopapa D, et al.: Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab 89 (2): 574-80, 2004. [PUBMED Abstract]
Stage Information for Pituitary Tumors
As with other tumors of the central nervous system (CNS), no TNM (tumor, node, metastasis)-based American Joint Committee on Cancer classification and staging system for pituitary tumors exists.[1] Pituitary tumors are classified according to size and divided into microadenomas (i.e., the greatest diameter is <10 mm) and macroadenomas (i.e., the greatest diameter is ≥10 mm).[2] Most pituitary adenomas are microadenomas.
The most widely used radioanatomical classification was based primarily on a neuroradiological examination including skull x-rays, pneumoencephalography, polytomography, and carotid angiography.[3] This radioanatomical classification was subsequently validated by more accurate magnetic resonance imaging (MRI) and computed tomography. It has been augmented by additional studies including immunohistochemistry and electron microscopy. The classification places adenomas into one of five grades (0–IV).[4]
Currently, MRI is considered the imaging modality of choice for the diagnosis of pituitary disorders because of its multiplanar capability and good soft tissue contrast enhancement.[2] Because no unequivocal histopathological features of pituitary carcinoma exist, the diagnosis of malignancy is reserved for pituitary neoplasms that have metastasized to remote areas of the CNS or to outside of the CNS.[5–7]
The radiographical classification for pituitary adenomas is as follows:[3,8]
- 0: Normal pituitary appearance.
- I: Enclosed within the sella turcica, microadenoma, smaller than 10 mm.
- II: Enclosed within the sella turcica, macroadenoma, 10 mm or larger.
- III: Invasive, locally, into the sella.
- IV: Invasive, diffusely, into the sella.
The grading schema for suprasellar extensions is as follows:[3,8]
- A: 0 to 10 mm suprasellar extension occupying the suprasellar cistern.
- B: 10 mm to 20 mm extension and elevation of the third ventricle.
- C: 20 mm to 30 mm extension occupying the anterior of the third ventricle.
- D: An extension larger than 30 mm, beyond the foramen of Monro, or Grade C with lateral extensions.
References
- Brain and Spinal Cord. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. Springer; 2017, pp. 857–69.
- Ezzat S, Asa SL, Couldwell WT, et al.: The prevalence of pituitary adenomas: a systematic review. Cancer 101 (3): 613-9, 2004. [PUBMED Abstract]
- Hardy J: Transsphenoidal surgery of hypersecreting pituitary tumors. In: Kohler PO, Ross GT, eds.: Diagnosis and treatment of pituitary tumors: proceedings of a conference sponsored jointly by the National Institute of Child Health and Human Development and the National Cancer Institute, January 15-17, 1973, Bethesda, Md. Amsterdam, The Netherlands: Excerpta medica, 1973, pp 179-98.
- Asa SL, Ezzat S: The cytogenesis and pathogenesis of pituitary adenomas. Endocr Rev 19 (6): 798-827, 1998. [PUBMED Abstract]
- Scheithauer BW, Kovacs KT, Laws ER, et al.: Pathology of invasive pituitary tumors with special reference to functional classification. J Neurosurg 65 (6): 733-44, 1986. [PUBMED Abstract]
- Della Casa S, Corsello SM, Satta MA, et al.: Intracranial and spinal dissemination of an ACTH secreting pituitary neoplasia. Case report and review of the literature. Ann Endocrinol (Paris) 58 (6): 503-9, 1997. [PUBMED Abstract]
- Kemink SA, Wesseling P, Pieters GF, et al.: Progression of a Nelson’s adenoma to pituitary carcinoma; a case report and review of the literature. J Endocrinol Invest 22 (1): 70-5, 1999. [PUBMED Abstract]
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
Treatment Option Overview for Pituitary Tumors
The goals of treatment of pituitary adenomas include normalization of hormonal secretion (i.e., normalization of hypersecretion and improvement in hypofunction) and resolution or cessation of the progression of neurological defects.
Treatment options for patients with pituitary tumors include:
- Surgery.
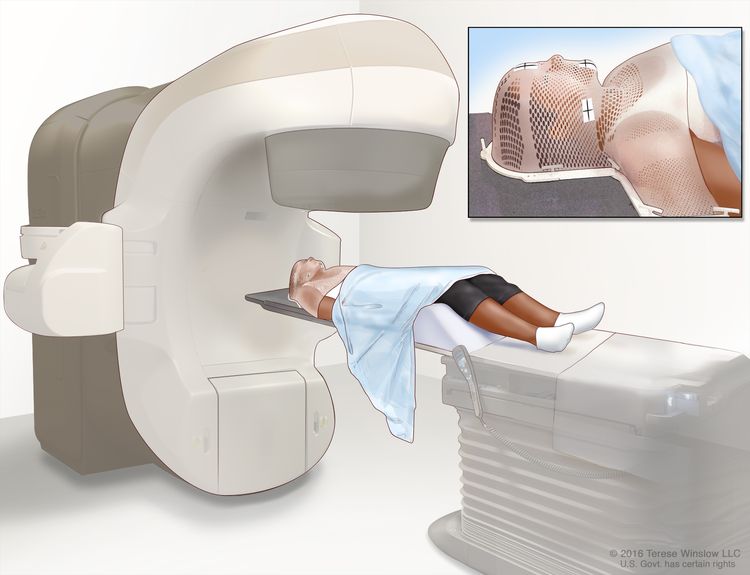
- Radiation therapy.
- Medical therapy.
- A combination of surgery, radiation therapy, and medical therapy.
- Stereotactic radiation surgery (under clinical evaluation).[1]
The choice of treatment must be individualized and is dictated by the type of tumor, the nature of the excessive hormonal expression, and whether the tumor extends into the brain around the pituitary.[2,3]
The transsphenoidal microsurgical approach to a pituitary lesion is the most widely used approach and represents a major development in the safe surgical treatment of both hormonally active and nonfunctioning tumors.[4–6] This approach is often successful in debulking tumors, even those that have a significant suprasellar extension.
This surgery is contraindicated in patients with tumors with a significant suprasellar extension and an hourglass-shaped narrowing between the intrasellar and suprasellar component because blind attempts to reach the suprasellar tumor may lead to cerebral damage. In addition, an infection in the sphenoid sinus is a potential contraindication to the transsphenoidal approach. In such cases, craniotomies via a pterional or subfrontal approach may be performed. Rapid deterioration of vision is an immediate indication for surgery to relieve pressure produced by an expanding tumor mass, except in the case of macroprolactinomas (where intensive observation with a patient on dopaminergic agonists may be an acceptable alternative). Progressive deterioration of visual fields is often the primary neurological criterion on which surgical management decisions are based.[7]
Conventional radiation therapy is an effective adjunct to the treatment of pituitary tumors.[4] The advantages of radiation therapy are that it is noninvasive and suitable for surgically high-risk patients. The clinical and biochemical response, however, is slow and may require from 2 to 10 years for complete and sustained remission. In addition, radiation therapy carries a substantial risk of hypopituitarism (i.e., approximately 30% at 10 years).
Hormone-secreting tumors may be treated with surgery or radiation therapy. Surgical therapy is the treatment of choice for growth hormone (GH)-producing, adrenocorticotropic hormone (ACTH)-producing, and endocrine-inactive adenomas. GH-secreting tumors can be treated with somatostatin analogues, dopamine analogues, and GH-receptor antagonists, such as pegvisomant.[7] Ketoconazole, an inhibitor of steroidogenesis, is considered the first drug of choice as adjuvant therapy for ACTH-producing tumors.[4] Somatostatin analogues are the treatment of choice for thyroid-stimulating hormone-producing adenomas, but their efficacy may wane with time.[7]
The natural history of GH-secreting and ACTH-secreting pituitary tumors is usually one of slowly progressive enlargement.[4] Microprolactinomas, however, often remain unchanged, or decrease in size over time, and they have occasionally been observed to undergo complete, spontaneous resolution.[7]
References
- Laws ER, Sheehan JP, Sheehan JM, et al.: Stereotactic radiosurgery for pituitary adenomas: a review of the literature. J Neurooncol 69 (1-3): 257-72, 2004 Aug-Sep. [PUBMED Abstract]
- Asa SL, Ezzat S: The cytogenesis and pathogenesis of pituitary adenomas. Endocr Rev 19 (6): 798-827, 1998. [PUBMED Abstract]
- Landman RE, Horwith M, Peterson RE, et al.: Long-term survival with ACTH-secreting carcinoma of the pituitary: a case report and review of the literature. J Clin Endocrinol Metab 87 (7): 3084-9, 2002. [PUBMED Abstract]
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
- Hardy J: Transsphenoidal microsurgery of the normal and pathological pituitary. Clin Neurosurg 16: 185-217, 1969. [PUBMED Abstract]
- Hardy J: Transsphenoidal hypophysectomy. J Neurosurg 34 (4): 582-94, 1971. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
Treatment of Prolactin-Producing Pituitary Tumors
Treatment Options for Prolactin (PRL)-Producing Pituitary Tumors
Treatment options for PRL-producing pituitary tumors include:
When the pituitary tumor secretes PRL, treatment depends on tumor size and the symptoms that result from excessive hormone production. Patients with PRL-secreting tumors are treated with surgery and radiation therapy.[1]
Most microprolactinomas and macroprolactinomas respond well to medical therapy with ergot-derived dopamine agonists, including bromocriptine and cabergoline.[2] For many patients, cabergoline has a more tolerable side effect profile than bromocriptine. Cabergoline therapy may be successful in treating patients whose prolactinomas are resistant to bromocriptine or who cannot tolerate bromocriptine, and this treatment has a success rate of more than 90% in patients with newly diagnosed prolactinomas.[3–5] In a prospective study, cabergoline was safely withdrawn in patients with normalized PRL levels and no evidence of tumor, which may produce a cure rate of approximately 70%.[6] Bromocriptine is the treatment of choice when the patient wants to preserve fertility because of its safety record in pregnancy.[7]
Microprolactinomas change little in size with treatment, but macroprolactinomas can shrink, sometimes quite dramatically. Microprolactinomas may decrease in size over time and they have occasionally been observed to undergo complete, spontaneous resolution.[8] Surgery is typically reserved for patients who cannot tolerate dopamine agonists, who suffer pituitary apoplexy during treatment, or whose macroprolactinomas are not responsive to medical therapy.[2] Occasionally, these tumors may require radiation therapy.[9]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
- Colao A, Di Sarno A, Landi ML, et al.: Macroprolactinoma shrinkage during cabergoline treatment is greater in naive patients than in patients pretreated with other dopamine agonists: a prospective study in 110 patients. J Clin Endocrinol Metab 85 (6): 2247-52, 2000. [PUBMED Abstract]
- Cannavò S, Curtò L, Squadrito S, et al.: Cabergoline: a first-choice treatment in patients with previously untreated prolactin-secreting pituitary adenoma. J Endocrinol Invest 22 (5): 354-9, 1999. [PUBMED Abstract]
- Colao A, Di Sarno A, Landi ML, et al.: Long-term and low-dose treatment with cabergoline induces macroprolactinoma shrinkage. J Clin Endocrinol Metab 82 (11): 3574-9, 1997. [PUBMED Abstract]
- Colao A, Di Sarno A, Cappabianca P, et al.: Withdrawal of long-term cabergoline therapy for tumoral and nontumoral hyperprolactinemia. N Engl J Med 349 (21): 2023-33, 2003. [PUBMED Abstract]
- Schlechte JA: Clinical practice. Prolactinoma. N Engl J Med 349 (21): 2035-41, 2003. [PUBMED Abstract]
- Ezzat S, Asa SL, Couldwell WT, et al.: The prevalence of pituitary adenomas: a systematic review. Cancer 101 (3): 613-9, 2004. [PUBMED Abstract]
- Nomikos P, Buchfelder M, Fahlbusch R: Current management of prolactinomas. J Neurooncol 54 (2): 139-50, 2001. [PUBMED Abstract]
Treatment of Adrenocorticotropic Hormone–Producing Pituitary Tumors
Treatment Options for Adrenocorticotropic Hormone (ACTH)–Producing Pituitary Tumors
Treatment options for ACTH-producing pituitary tumors include:
Transsphenoidal microsurgery is the treatment of choice for patients with corticotroph adenomas.[1,2] Most series report remission rates of approximately 70% to 90%.[1] In a series of 216 patients who underwent surgery using a transsphenoidal approach, 75% experienced long-term remission, 21% experienced persistence of Cushing disease, and 9% had recurrence after the initial correction of the hypercortisolism.[3] The average time interval for reoperation was 3.8 years. Seventy-nine percent of the tumors were microadenomas, and 18% were macroadenomas; 86% of the cases with microadenoma had long-term remission, compared with only 46% of those with macroadenoma. In cases in which hypercortisolemia persists, early repeat exploration and/or radiation therapy or laparoscopic bilateral adrenalectomy may be required.[2]
Radiation therapy has been used in patients who are not surgical candidates and has also been used as adjuvant therapy in patients with residual or recurrent active tumor.[1,4]
Drug therapy may be an adjunct to transsphenoidal microsurgery in cases of residual tumor and in cases where radiation therapy has a delayed effect.[1] Steroidogenesis inhibitors, including mitotane, metyrapone, ketoconazole, and aminoglutethimide are used. Ketoconazole is the best tolerated of these agents and is effective as monotherapy in about 70% of patients.[5]
If untreated, patients frequently die of cardiovascular disease or infection.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
- Mampalam TJ, Tyrrell JB, Wilson CB: Transsphenoidal microsurgery for Cushing disease. A report of 216 cases. Ann Intern Med 109 (6): 487-93, 1988. [PUBMED Abstract]
- Mahmoud-Ahmed AS, Suh JH: Radiation therapy for Cushing’s disease: a review. Pituitary 5 (3): 175-80, 2002. [PUBMED Abstract]
- Nieman LK: Medical therapy of Cushing’s disease. Pituitary 5 (2): 77-82, 2002. [PUBMED Abstract]
- Devin JK, Allen GS, Cmelak AJ, et al.: The efficacy of linear accelerator radiosurgery in the management of patients with Cushing’s disease. Stereotact Funct Neurosurg 82 (5-6): 254-62, 2004. [PUBMED Abstract]
- Wong GK, Leung CH, Chiu KW, et al.: LINAC radiosurgery in recurrent Cushing’s disease after transsphenoidal surgery: a series of 5 cases. Minim Invasive Neurosurg 46 (6): 327-30, 2003. [PUBMED Abstract]
Treatment of Growth Hormone–Producing Pituitary Tumors
Treatment Options for Growth Hormone (GH)–Producing Pituitary Tumors
Treatment options for GH-producing pituitary tumors include:
Treatment for patients with acromegaly includes surgical, radiation, and medical therapies.[3] Treatment depends on the size and extent of the tumor and the need for rapid cessation of hormone function that results in serious clinical sequelae (i.e., hypertension and cardiomyopathy).
Microadenomectomy or macroadenoma decompression is approached transsphenoidally in most patients. Increasingly, endoscopic surgery is used to allow the entire surgical field to be viewed and to allow tumor tissue that would otherwise be inaccessible with rigid instruments to be safely resected. However, normalization of GH levels is not often achieved. Increasingly, adjuvant radiation therapy is reserved for tumors that extend beyond the safe operative area and appear to pose an ongoing threat.
Drug treatment, whether used as an adjuvant or primary therapy in appropriately selected patients,[4] includes the use of somatostatin analogues, such as octreotide; dopamine analogues, such as bromocriptine; and, the GH-receptor antagonist pegvisomant. As the first of a new class of GH-receptor antagonists, pegvisomant works by inhibiting functional dimerization of GH receptors, inhibiting GH action. Results indicate that it may be the most effective medical treatment for acromegaly.[1,2]
In acromegalic patients, impaired glucose tolerance, hypertension, and hyperlipidemia should be vigorously treated concurrently with definitive therapy. A multidisciplinary clinical approach may be required for the treatment of arthritis, carpal tunnel syndrome, obstructive sleep apnea, and prognathism.[5] Mortality is related primarily to cardiovascular and respiratory diseases.[5]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Stewart PM: Pegvisomant: an advance in clinical efficacy in acromegaly. Eur J Endocrinol 148 (Suppl 2): S27-32, 2003. [PUBMED Abstract]
- Muller AF, Kopchick JJ, Flyvbjerg A, et al.: Clinical review 166: Growth hormone receptor antagonists. J Clin Endocrinol Metab 89 (4): 1503-11, 2004. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
- Kleinberg DL: Primary therapy for acromegaly with somatostatin analogs and a discussion of novel peptide analogs. Rev Endocr Metab Disord 6 (1): 29-37, 2005. [PUBMED Abstract]
- Colao A, Ferone D, Marzullo P, et al.: Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 25 (1): 102-52, 2004. [PUBMED Abstract]
Treatment of Thyrotropin-Producing Tumors
Treatment Options for Thyrotropin-Producing Tumors
Treatment options for thyrotropin-producing tumors include:
Transsphenoidal surgery is the treatment of choice for patients with thyrotropic adenomas.[1] Adjuvant radiation therapy may be used when surgery is known to be noncurative, even if the patient is still euthyroid. This is because relapse is inevitable, and the full effect of radiation therapy requires months or years.
Medical therapy may be required for patients who still have hyperthyroid symptoms despite surgery and external radiation. Somatostatin analogues are the treatment of choice, but their efficacy may wane with time.[1–4]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Brucker-Davis F, Oldfield EH, Skarulis MC, et al.: Thyrotropin-secreting pituitary tumors: diagnostic criteria, thyroid hormone sensitivity, and treatment outcome in 25 patients followed at the National Institutes of Health. J Clin Endocrinol Metab 84 (2): 476-86, 1999. [PUBMED Abstract]
- Levy A: Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry 75 (Suppl 3): iii47-52, 2004. [PUBMED Abstract]
- Caron P, Arlot S, Bauters C, et al.: Efficacy of the long-acting octreotide formulation (octreotide-LAR) in patients with thyrotropin-secreting pituitary adenomas. J Clin Endocrinol Metab 86 (6): 2849-53, 2001. [PUBMED Abstract]
- Teramoto A, Sanno N, Tahara S, et al.: Pathological study of thyrotropin-secreting pituitary adenoma: plurihormonality and medical treatment. Acta Neuropathol (Berl) 108 (2): 147-53, 2004. [PUBMED Abstract]
Treatment of Nonfunctioning Pituitary Tumors
Treatment Options for Nonfunctioning Pituitary Tumors
Treatment options for nonfunctioning pituitary tumors include:
Treatment selection for patients with nonfunctioning (endocrine-inactive) tumors depends on tumor size, the progressive course of the disease, and anatomical structures affected by the tumor extension. Most patients present with suprasellar extension and visual field deficits. In addition, many have hormone deficits before treatment. The initial treatment of patients with gonadotroph adenomas is usually by transsphenoidal surgery, particularly if the adenoma presents with neurological symptoms. This is because the effect of radiation therapy occurs too slowly, and no reliable medical therapy exists.[4]
The first choice of treatment for patients with endocrine-inactive pituitary adenomas is usually surgery, which ameliorates symptoms of chiasmal compression and headache.[1] However, radical removal of the tumor is difficult because of frequent invasion into the cavernous sinus. Seventy percent to 80% of patients experience normalization or improvement of visual field defects, and almost 100% of patients with headache as a presenting symptom experience relief. Regrowth of the tumor after radiologically confirmed gross total removal appears to be uncommon. In a series of 32 patients, only 2 (6.2%) with gross total tumor removal and no postoperative radiation therapy showed radiological recurrence of the tumor at a mean follow-up of 5.5 years.[5]
Radiation therapy has been given postoperatively, and after clear radiological evidence of residual or recurrent tumor has been demonstrated.[1–3] Drug therapy appears to be of limited value.[1–3]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Losa M, Mortini P, Barzaghi R, et al.: Endocrine inactive and gonadotroph adenomas: diagnosis and management. J Neurooncol 54 (2): 167-77, 2001. [PUBMED Abstract]
- Yeh PJ, Chen JW: Pituitary tumors: surgical and medical management. Surg Oncol 6 (2): 67-92, 1997. [PUBMED Abstract]
- Tsang RW, Brierley JD, Panzarella T, et al.: Radiation therapy for pituitary adenoma: treatment outcome and prognostic factors. Int J Radiat Oncol Biol Phys 30 (3): 557-65, 1994. [PUBMED Abstract]
- Snyder PJ: Extensive personal experience: gonadotroph adenomas. J Clin Endocrinol Metab 80 (4): 1059-61, 1995. [PUBMED Abstract]
- Lillehei KO, Kirschman DL, Kleinschmidt-DeMasters BK, et al.: Reassessment of the role of radiation therapy in the treatment of endocrine-inactive pituitary macroadenomas. Neurosurgery 43 (3): 432-8; discussion 438-9, 1998. [PUBMED Abstract]
Treatment of Pituitary Carcinomas
Treatment Options for Pituitary Carcinomas
Treatment options for pituitary carcinomas include:
- Surgery.
- Dopamine agonists, such as bromocriptine, pergolide, quinagolide, and cabergoline, for prolactin (PRL)-producing carcinomas.
- Somatostatin analogues, such as octreotide, for growth hormone (GH)–producing and thyroid-stimulating hormone (TSH)-producing carcinomas.
- Adjuvant radiation therapy, which does not appear to change outcome.
- Chemotherapy, which is of little benefit.
Some reports indicate that as many as 88% of pituitary carcinomas are endocrinologically active, and adrenocorticotrophin hormone-secreting tumors are the most common.[1] Treatments for patients with pituitary carcinomas are palliative, with the mean survival time ranging from 2 to 2.4 years, though several case reports of long-term survivors have been published.[2–5]
Treatment options for patients with pituitary carcinomas include resection and dopamine agonists for PRL-producing tumors; somatostatin analogues for GH-producing and TSH-producing tumors; radiation therapy, and chemotherapy.[1]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Ragel BT, Couldwell WT: Pituitary carcinoma: a review of the literature. Neurosurg Focus 16 (4): E7, 2004. [PUBMED Abstract]
- Pernicone PJ, Scheithauer BW, Sebo TJ, et al.: Pituitary carcinoma: a clinicopathologic study of 15 cases. Cancer 79 (4): 804-12, 1997. [PUBMED Abstract]
- Sironi M, Cenacchi G, Cozzi L, et al.: Progression on metastatic neuroendocrine carcinoma from a recurrent prolactinoma: a case report. J Clin Pathol 55 (2): 148-51, 2002. [PUBMED Abstract]
- Landman RE, Horwith M, Peterson RE, et al.: Long-term survival with ACTH-secreting carcinoma of the pituitary: a case report and review of the literature. J Clin Endocrinol Metab 87 (7): 3084-9, 2002. [PUBMED Abstract]
- Vaquero J, Herrero J, Cincu R: Late development of frontal prolactinoma after resection of pituitary tumor. J Neurooncol 64 (3): 255-8, 2003. [PUBMED Abstract]
Treatment of Recurrent Pituitary Tumors
Treatment Options for Recurrent Pituitary Tumors
Treatment options for recurrent pituitary tumors include:
Treatment for patients with relapsed disease depends on many factors, including the specific type of pituitary tumor, previous treatment, visual and hormonal complications, and individual patient considerations.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Kovalic JJ, Grigsby PW, Fineberg BB: Recurrent pituitary adenomas after surgical resection: the role of radiation therapy. Radiology 177 (1): 273-5, 1990. [PUBMED Abstract]
- Tsang RW, Brierley JD, Panzarella T, et al.: Radiation therapy for pituitary adenoma: treatment outcome and prognostic factors. Int J Radiat Oncol Biol Phys 30 (3): 557-65, 1994. [PUBMED Abstract]
- Schoenthaler R, Albright NW, Wara WM, et al.: Re-irradiation of pituitary adenoma. Int J Radiat Oncol Biol Phys 24 (2): 307-14, 1992. [PUBMED Abstract]
- Sheehan JP, Kondziolka D, Flickinger J, et al.: Radiosurgery for residual or recurrent nonfunctioning pituitary adenoma. J Neurosurg 97 (5 Suppl): 408-14, 2002. [PUBMED Abstract]
- Laws ER, Sheehan JP, Sheehan JM, et al.: Stereotactic radiosurgery for pituitary adenomas: a review of the literature. J Neurooncol 69 (1-3): 257-72, 2004 Aug-Sep. [PUBMED Abstract]
- Picozzi P, Losa M, Mortini P, et al.: Radiosurgery and the prevention of regrowth of incompletely removed nonfunctioning pituitary adenomas. J Neurosurg 102 (Suppl): 71-4, 2005. [PUBMED Abstract]
Latest Updates to This Summary (12/17/2024)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Editorial changes were made to this summary.
This summary is written and maintained by the PDQ Adult Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of pituitary tumors. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Adult Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Pituitary Tumors Treatment are:
- Solmaz Sahebjam, MD (Johns Hopkins at Sibley Memorial Hospital)
- Minh Tam Truong, MD (Boston University Medical Center)
- Jaydira del Rivero, MD (National Cancer Institute)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website’s Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Adult Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Pituitary Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: /types/pituitary/hp/pituitary-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389459]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
Based on the strength of the available evidence, treatment options may be described as either “standard” or “under clinical evaluation.” These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.