Childhood Chronic Myeloid Leukemia Treatment (PDQ®)–Health Professional Version
Incidence and Clinical Presentation
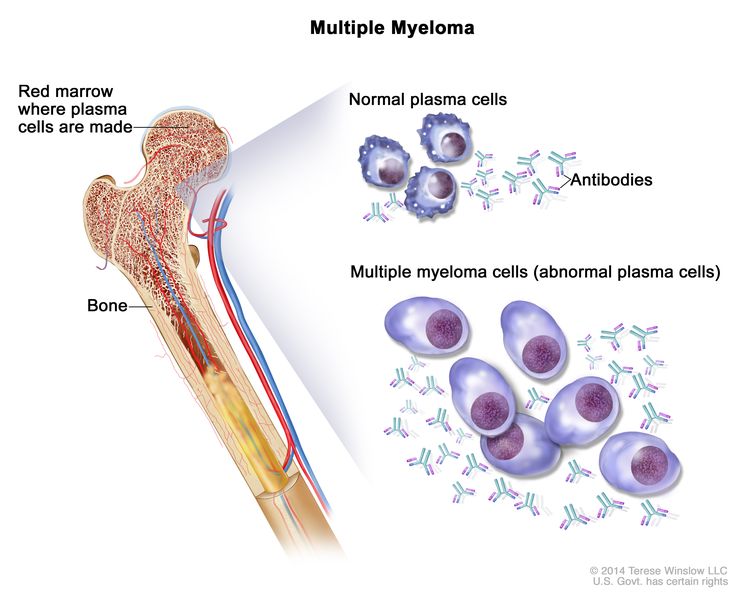
Chronic myeloid leukemia (CML) results from the BCR::ABL1 translocation. CML is primarily an adult disease but represents the most common of the chronic myeloproliferative disorders in children. CML accounts for approximately 13% to 20% of all childhood myeloid leukemias and 2% of all childhood leukemias.[1–4] Although it has been reported in very young children, most patients are aged 6 years and older. CML most commonly occurs in older adolescents.
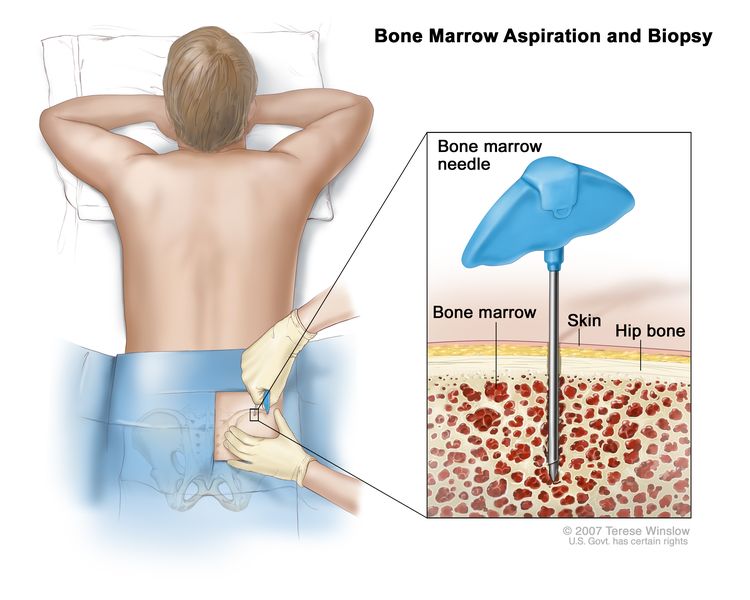
CML is a clonal panmyelopathy that involves all hematopoietic cell lineages. CML is characterized by a marked leukocytosis and is often associated with thrombocytosis, sometimes with abnormal platelet function. Bone marrow aspiration or biopsy reveals hypercellularity with relatively normal granulocytic maturation and no significant increase in leukemic blasts. Although reduced leukocyte alkaline phosphatase activity is seen in patients with CML, this is not a specific finding.
CML historically was divided into the following three clinical phases:
- Chronic phase. Chronic phase, which lasts for approximately 3 years if untreated, usually presents with symptoms secondary to hyperleukocytosis such as weakness, fever, night sweats, bone pain, respiratory distress, priapism, left upper quadrant pain (splenomegaly), and, rarely, hearing loss and visual disturbances.
- Accelerated phase. This phase is now omitted in the 5th edition of the World Health Organization (WHO) Classification of Hematolymphoid Tumors.[5,6] It was previously defined by progressive splenomegaly, thrombocytopenia, and increased percentage of peripheral and bone marrow blasts, along with accumulation of karyotypic abnormalities in addition to the Philadelphia (Ph) chromosome. However, in the era of using tyrosine kinase inhibitors (TKIs), this phase is less prognostically relevant.
- Blast crisis phase. Blast crisis is notable for the bone marrow showing greater than 20% blasts or chloromatous lesions or the presence of increased lymphoblasts (even if <10%) in peripheral blood or bone marrow. The clinical picture of CML is indistinguishable from acute leukemia. Approximately two-thirds of blast crisis is myeloid, and the remainder is lymphoid, usually of B lineage. Patients in blast crisis will die within a few months.[7]
The 5th edition of the WHO classification now divides clinical presentation into either chronic phase or blast phase and eliminates the accelerated phase. This change was partially due to the impact of TKIs on the disease course, which has reduced the proportion of patients who develop progression. Also, the 5th edition of the WHO classification identifies certain chronic phase characteristics as high risk for disease progression and TKI resistance.[6] These characteristics, present at diagnosis or during TKI therapy, include the following:
- High-risk features of chronic-phase CML at diagnosis include the following:
- High European Treatment and Outcome Study (EUTOS) long-term survival (ELTS) score.
- Ten percent to 19% myeloid blasts in the peripheral blood or bone marrow. Presence of lymphoblasts in the peripheral blood or bone marrow (even if <10%) is indicative of blast crisis–phase disease.
- Basophils of 20% or higher in the peripheral blood.
- Additional chromosomal aberrations in Ph chromosome–positive (Ph+) cells (3q26.2 rearrangements, monosomy 7, isochromosome 17q, and/or complex karyotypes). Other aberrations include trisomy 8, 11q23 rearrangements, trisomy 19, trisomy 21, additional Ph+ in Ph+ cells, although the evidence of association with disease progression is less clear.
- Clusters of small megakaryocytes associated with significant bone marrow fibrosis (MF2-3).
- High-risk features of chronic-phase CML during treatment with TKIs include the following:
- Failure to achieve a complete hematologic response to the first TKI.
- Development of hematologic, cytogenetic, or molecular indications of resistance to two sequential TKIs.
- Development of new additional chromosomal abnormalities and/or occurrence of compound variants (≥2 variants in the same BCR::ABL1 molecule) in the BCR::ABL1 fusion gene during TKI therapy.
References
- Ries LA, Smith MA, Gurney JG, et al., eds.: Cancer incidence and survival among children and adolescents: United States SEER Program 1975-1995. National Cancer Institute, SEER Program, 1999. NIH Pub.No. 99-4649. Also available online. Last accessed December 22, 2023.
- Surveillance Research Program, National Cancer Institute: SEER*Explorer: An interactive website for SEER cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed December 30, 2024.
- National Cancer Institute: NCCR*Explorer: An interactive website for NCCR cancer statistics. Bethesda, MD: National Cancer Institute. Available online. Last accessed February 25, 2025.
- Mattano L Jr, Nachman J, Ross J, et al.: Leukemias. In: Bleyer A, O’Leary M, Barr R, et al., eds.: Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. National Cancer Institute, 2006. NIH Pub. No. 06-5767., pp 39-52.
- Khoury JD, Solary E, Abla O, et al.: The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia 36 (7): 1703-1719, 2022. [PUBMED Abstract]
- Loghavi S, Kanagal-Shamanna R, Khoury JD, et al.: Fifth Edition of the World Health Classification of Tumors of the Hematopoietic and Lymphoid Tissue: Myeloid Neoplasms. Mod Pathol 37 (2): 100397, 2024. [PUBMED Abstract]
- O’Dwyer ME, Mauro MJ, Kurilik G, et al.: The impact of clonal evolution on response to imatinib mesylate (STI571) in accelerated phase CML. Blood 100 (5): 1628-33, 2002. [PUBMED Abstract]
Cytogenetics of CML
Genomics of CML
The cytogenetic abnormality required for diagnosis of CML is the Philadelphia chromosome (Ph), which represents a translocation of chromosomes 9 and 22 (t(9;22)), resulting in a BCR::ABL1 fusion protein.[1]
Additional chromosomal abnormalities have been found in studies of adults with CML in the TKI era. These studies have illustrated a number of adverse prognostic variants, including those identified as high risk in the chronic phase.[2,3]
References
- Quintás-Cardama A, Cortes J: Molecular biology of bcr-abl1-positive chronic myeloid leukemia. Blood 113 (8): 1619-30, 2009. [PUBMED Abstract]
- Loghavi S, Kanagal-Shamanna R, Khoury JD, et al.: Fifth Edition of the World Health Classification of Tumors of the Hematopoietic and Lymphoid Tissue: Myeloid Neoplasms. Mod Pathol 37 (2): 100397, 2024. [PUBMED Abstract]
- Wang W, Cortes JE, Tang G, et al.: Risk stratification of chromosomal abnormalities in chronic myelogenous leukemia in the era of tyrosine kinase inhibitor therapy. Blood 127 (22): 2742-50, 2016. [PUBMED Abstract]
Special Considerations for the Treatment of Children With Cancer
Cancer in children and adolescents is rare, although the overall incidence has slowly increased since 1975.[1] Children and adolescents with cancer should be referred to medical centers that have a multidisciplinary team of cancer specialists with experience treating the cancers that occur during childhood and adolescence.[2] This multidisciplinary team approach incorporates the skills of the following pediatric specialists and others to ensure that children receive treatment, supportive care, and rehabilitation to achieve optimal survival and quality of life:
- Primary care physicians.
- Pediatric surgeons.
- Pathologists.
- Pediatric radiation oncologists.
- Pediatric medical oncologists and hematologists.
- Rehabilitation specialists.
- Pediatric oncology nurses.
- Social workers.
- Child-life professionals.
- Psychologists.
- Nutritionists.
For specific information about supportive care for children and adolescents with cancer, see the summaries on Supportive and Palliative Care.
The American Academy of Pediatrics has outlined guidelines for pediatric cancer centers and their role in the treatment of children and adolescents with cancer.[3] At these centers, clinical trials are available for most types of cancer that occur in children and adolescents, and the opportunity to participate is offered to most patients and their families. Clinical trials for children and adolescents diagnosed with cancer are generally designed to compare potentially better therapy with current standard therapy. Other types of clinical trials test novel therapies when there is no standard therapy for a cancer diagnosis. Most of the progress in identifying curative therapies for childhood cancers has been achieved through clinical trials. Information about ongoing clinical trials is available from the NCI website.
References
- Smith MA, Seibel NL, Altekruse SF, et al.: Outcomes for children and adolescents with cancer: challenges for the twenty-first century. J Clin Oncol 28 (15): 2625-34, 2010. [PUBMED Abstract]
- Wolfson J, Sun CL, Wyatt L, et al.: Adolescents and Young Adults with Acute Lymphoblastic Leukemia and Acute Myeloid Leukemia: Impact of Care at Specialized Cancer Centers on Survival Outcome. Cancer Epidemiol Biomarkers Prev 26 (3): 312-320, 2017. [PUBMED Abstract]
- American Academy of Pediatrics: Standards for pediatric cancer centers. Pediatrics 134 (2): 410-4, 2014. Also available online. Last accessed February 25, 2025.
Historical (Pre–Tyrosine Kinase Inhibitor) Therapy for Childhood CML
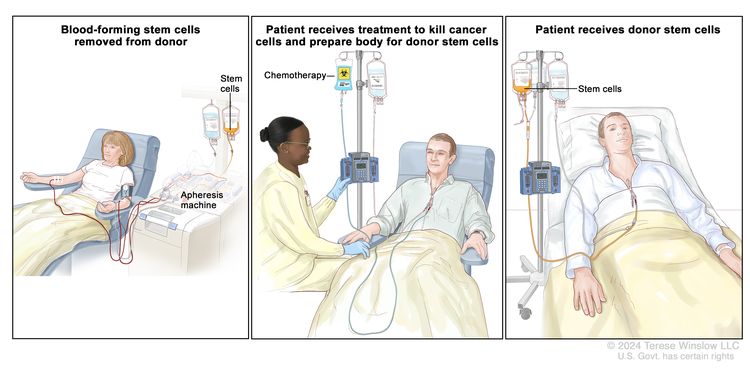
Before the tyrosine kinase inhibitor (TKI) era, allogeneic hematopoietic stem cell transplant (HSCT) was the primary treatment for children with chronic myeloid leukemia (CML). Published reports from this period described survival rates of 70% to 80% when an HLA–matched-family donor (MFD) was used in the treatment of children in early chronic phase. Lower survival rates were reported when HLA–matched-unrelated donors were used.[1–3]
Relapse rates were low (less than 20%) when transplant was performed in the chronic phase.[1,2] The primary cause of death was treatment-related mortality, which was increased with HLA–matched-unrelated donors compared with HLA-MFDs in most reports.[1,2] High-resolution DNA matching for HLA alleles appeared to reduce rates of treatment-related mortality, leading to improved outcome for HSCT using unrelated donors.[4]
Compared with transplant in the chronic phase, transplant in the accelerated phase or blast crisis and in the second chronic phase resulted in significantly reduced survival.[1–3] The use of T-lymphocyte depletion to avoid graft-versus-host disease resulted in a higher relapse rate and decreased overall survival,[5] supporting the contribution of a graft-versus-leukemia effect to favorable outcome after allogeneic HSCT.
The introduction of the TKI imatinib as a therapeutic drug targeted at inhibiting the BCR::ABL1 fusion kinase revolutionized the treatment of patients with CML, for both children and adults.[6] Most data on the use of TKIs for CML are from adult clinical trials. For more information, see Chronic Myeloid Leukemia Treatment. The more limited experience in children is described below.
References
- Millot F, Esperou H, Bordigoni P, et al.: Allogeneic bone marrow transplantation for chronic myeloid leukemia in childhood: a report from the Société Française de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC). Bone Marrow Transplant 32 (10): 993-9, 2003. [PUBMED Abstract]
- Cwynarski K, Roberts IA, Iacobelli S, et al.: Stem cell transplantation for chronic myeloid leukemia in children. Blood 102 (4): 1224-31, 2003. [PUBMED Abstract]
- Weisdorf DJ, Anasetti C, Antin JH, et al.: Allogeneic bone marrow transplantation for chronic myelogenous leukemia: comparative analysis of unrelated versus matched sibling donor transplantation. Blood 99 (6): 1971-7, 2002. [PUBMED Abstract]
- Lee SJ, Klein J, Haagenson M, et al.: High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood 110 (13): 4576-83, 2007. [PUBMED Abstract]
- Horowitz MM, Gale RP, Sondel PM, et al.: Graft-versus-leukemia reactions after bone marrow transplantation. Blood 75 (3): 555-62, 1990. [PUBMED Abstract]
- Druker BJ: Translation of the Philadelphia chromosome into therapy for CML. Blood 112 (13): 4808-17, 2008. [PUBMED Abstract]
Treatment of Childhood CML
Treatment options for children with chronic myeloid leukemia (CML) may include the following:
- Tyrosine kinase inhibitor (TKI) therapy.
TKI Therapy
An increasing number of targeted agents are now approved for use in adults with CML. The use of these agents in pediatric patients is slow because there are not many studies that include children. Table 1 and the following narratives describe findings from specific trials where pediatric data are available.
| Target and Agents | Prospective Pediatric Outcomes | Reference | ||||
|---|---|---|---|---|---|---|
| CHR | CCyR | MMR | PFS | |||
| ATP = adenosine triphosphate; CHR = complete hematologic response; CCyR = complete cytogenetic response; MMR = major molecular response; PFS = progression-free survival. | ||||||
| aAt 36 months. | ||||||
| bAt 12 months. | ||||||
| cAt 48 months. | ||||||
| dFor available active clinical trials using this agent, see the Treatment Options Under Clinical Evaluation section. | ||||||
| BCR::ABL1 kinase domain ATP-binding pocket: | ||||||
| Imatinib 260 mg/m2 | 98%a | 61% | 31%b | 98% | Giona et al.[1] | |
| Imatinib 340 mg/m2 | 91.5% | 66.6%b | Giona et al.[1] | |||
| Dasatinib 60–72 mg/m2 | 92%b | 52%b | 93%c | Gore et al.[2] | ||
| Nilotinib 230 mg/m2 | 64%b | Hijiya et al.[3] | ||||
| Bosutinib 400 mg/m2 | Phase I study only | Brivio et al.[4] | ||||
| Ponatinibd | Anecdotal data only | |||||
| BCR::ABL1 kinase domain myristoyl-binding pocket: | ||||||
| Asciminibd | No prospective pediatric data | |||||
Imatinib
Imatinib has shown a high level of activity in children with CML that is comparable with the activity observed in adults.[1,5–8] As a result of this high level of activity, it is common to initiate imatinib treatment in children with CML rather than proceeding immediately to allogeneic stem cell transplant.[9] The pharmacokinetics of imatinib in children appear consistent with previous results in adults.[10]
Doses of imatinib used in phase II trials for children with CML have ranged from 260 mg/m2 to 340 mg/m2, which provide comparable drug exposures as the adult flat-doses of 400 mg to 600 mg.[1,7,8]
Evidence (imatinib in children):
- In a prospective trial, 44 pediatric patients with newly diagnosed CML were treated with imatinib (260 mg/day).[1]
- The progression-free survival (PFS) rate was 98% at 36 months.
- A complete hematologic response was achieved in 98% of the patients.
- The rate of complete cytogenetic response was 61%, and the rate of major molecular response was 31% at 12 months. These are similar to the rates seen in adult patients with chronic-phase CML who were treated with imatinib.
- In an Italian study, 47 pediatric patients with chronic-phase CML were treated with 340 mg/m2 per day of imatinib.[1]
- Complete cytogenetic response was achieved in 91.5% of patients at a median time of 6 months.
- The rate of major molecular response (MMR) at 12 months was 66.6%.
- Thus, it appears that starting with the higher dose of 340 mg/m2 has superior efficacy and is typically tolerable, with dose adjustment as needed for toxicity.[1,8]
Early molecular responses, such as the polymerase chain reaction (PCR)–based minimal residual disease (MRD) measurement at 3 months of therapy showing 10% BCR::ABL1 fusion transcripts, have been reported to be associated with improved PFS, similar to early molecular response data in adults.[11] The European LeukemiaNet (ELN) has defined optimal molecular milestones of BCR::ABL1 transcript levels to be 10% or less at 3 months, 1% or less at 6 months, and 0.1% or less at 12 months or more of therapy.[12]
The monitoring parameters described for adults with CML are reasonable to use in children. Monitoring occurs every 3 months until MMR is achieved and confirmed every 3 to 6 months thereafter. For more information, see Chronic Myeloid Leukemia Treatment.
Imatinib is generally well tolerated in children. Adverse effects are generally mild to moderate and reversible with treatment discontinuation or dose reduction.[7,8] Growth delay occurs in most prepubertal children who receive imatinib.[13] Children who receive imatinib and experience growth impairment may show some catch-up growth during their pubertal growth spurts, but they are at risk of having lower-than-expected adult height, as most patients do not achieve midparental height.[13,14]
Dasatinib
Dasatinib is a TKI that is approved by the U.S. Food and Drug Administration (FDA) for the treatment of children with CML.
Evidence (dasatinib in children):
- A phase I trial of dasatinib in children showed that drug disposition, tolerability, and efficacy of this agent was similar to that observed in adults.[15,16]
- A phase II trial of dasatinib, which included 84 children with newly diagnosed CML in chronic phase, used a dose of 60 mg/m2 (tablets) or 72 mg/m2 (oral solution) given to patients once daily.[2]
- Complete cytogenetic response and MMR (≥3-log reduction or ≤0.1% on the International Scale [IS]) were achieved in 92% and 52% of patients, respectively, after 12 months of therapy.
- The 4-year PFS rate was 93%.
- Dasatinib was well tolerated, with very few grade 3 or grade 4 adverse events. No pleural or pericardial effusions or pulmonary complications were observed.
Nilotinib
Nilotinib is a TKI that is approved by the FDA for the treatment of children with CML.
Evidence (nilotinib in children):
The FDA approved nilotinib in March 2018 for the treatment of children with CML based on two sponsored trials.[3,17]
- An initial study (NCT01077544 [CAMN107A2120]) of 11 patients evaluated pharmacokinetic, safety, and preliminary efficacy data.
- A second study (NCT01844765 [CAMN107A2203; AAML1321]) of 58 patients evaluated efficacy and safety.[3]
Data from both studies were combined for a pooled-data analysis of 69 patients, which included 25 patients with newly diagnosed CML and 44 patients with resistant or intolerant CML. Both studies used a dose of 230 mg/m2 given twice daily (rounded to the nearest 50 mg; maximum single dose, 400 mg).[3,17]
- In the phase II trial, 64% of patients with newly diagnosed CML achieved an MMR at 1 year.
- The tolerability of nilotinib in children was similar to that observed in adults. Primary side effects affecting more than 30% of children included headache, fever, and hyperbilirubinemia.
- Prolongation of QTc interval (defined in this trial as an increase of >30 msec over baseline) is a recognized side effect of nilotinib, and it was observed in 25% of children in these trials. The investigators recommended obtaining an electrocardiogram at baseline, 1 week, periodically afterward, and after dose adjustments.
Other TKIs
Most data on the use of TKIs for CML is from adult clinical trials. A safe pediatric dose has not yet been established for ponatinib.
Bosutinib is a TKI that targets the BCR::ABL1 gene fusion. The FDA approved bosutinib for the treatment of all phases of CML in adults who show intolerance to or whose disease shows resistance to previous therapy with another TKI.
The pediatric recommended phase II dose of bosutinib was determined in a phase I study that included 30 screened children, 28 of whom received treatment. For children previously resistant or intolerant to other TKIs, the dose was 400 mg/m2 with food once daily (maximum dose, 600 mg). For children with newly diagnosed CML, the dose was 300 mg/m2 with food once daily (maximum dose, 500 mg).[4]
- The most prevalent adverse event (all grades) was diarrhea, which occurred in 93% of the patients, 11% of whom had grade 3 or higher severity. In some cases, the diarrhea persisted for over 1 year of treatment.
- Additional adverse events of all grades (although most were grades 1–2) that occurred in over 50% of the children included nausea, vomiting, and abdominal pain.
- Fifteen children discontinued use of the agent (7 were intolerant and 8 had an inadequate response).
- Responses to bosutinib were considered similar to other TKIs.
Ponatinib is a BCR::ABL1 fusion transcript inhibitor that is effective against the T315I variant.[18] Ponatinib induced objective responses in approximately 70% of heavily pretreated adults with chronic-phase CML. Responses were observed regardless of the baseline BCR::ABL1 kinase domain variant.[19] The use of ponatinib has been complicated by the high rate of vascular occlusion observed in patients receiving the agent. Arterial and venous thrombosis and occlusions (including myocardial infarction and stroke) occurred in more than 20% of treated patients.[20] Ponatinib is being prospectively studied in the pediatric population.
Asciminib is an allosteric inhibitor of the myristoyl-binding pocket, whereas the previously described TKI agents target the adenosine triphosphate (ATP)–binding pocket. Asciminib was initially used to treat adults with CML that had developed resistance to the ATP-binding pocket agents.[21] Asciminib was effective in this setting, and the FDA approved it to treat CML with the T315I variant.[22] Subsequently, asciminib was approved to treat adults with newly diagnosed CML because MMR, as well as time to MMR, was significantly better with asciminib than with imatinib, and it trended similarly compared with second-generation TKIs. Safety profiles were also better with asciminib.[23] To date, there are no prospectively reported pediatric data for asciminib.
Discontinuation of TKI Therapy
Discontinuation of TKI treatment is an accepted strategy for adults with CML who meet strict criteria related to their duration of treatment and response to treatment. Guidelines for discontinuation of TKIs have been developed by both the ELN and the U.S.-based National Comprehensive Cancer Network (NCCN).[12,24] Key elements for both guidelines include the following:
- TKI therapy for a minimum duration of 4 to 5 years for ELN and 3 years for NCCN.
- A minimum duration of deep molecular response (DMR or MR4) (BCR::ABL1 protein transcript level ≤0.01% IS) of 2 years for both ELN and NCCN.
These guidelines specify close monitoring of BCR::ABL1 transcript levels after TKI discontinuation. Loss of MMR (or MR3) (BCR::ABL1 transcript level ≤0.1% IS) is generally used as the trigger for reinitiation of TKI therapy.
Loss of MMR is most likely to occur within the first 6 months of TKI discontinuation. Loss of MMR occurs much less frequently more than 1 year after TKI discontinuation. A meta-analysis included 3,105 adult patients who initiated a first attempt at TKI discontinuation. The study found that the probability of molecular recurrence was 35% after 0 to 6 months, 8% after 6 to 12 months, 3% after 12 to 18 months, and 3% after 18 to 24 months.[25] These results indicated that approximately 50% of adult patients maintained their molecular responses 2 years after TKI discontinuation. Relapses can occur when TKIs have been discontinued for more than 2 years, but these recurrences appear to be infrequent (<2%). Unfavorable outcomes were uncommon when relapses occurred. In addition, 90% of patients reacquired deep molecular remission after TKI reinitiation.
There are limited data regarding TKI discontinuation in children with CML. This limited experience is explained, in part, by the low incidence of CML in children. In addition, few children with CML who are treated with TKIs meet the criteria for TKI discontinuation. For example, among patients enrolled on the International Chronic Myeloid Leukemia Pediatric Study (I-CML-Ped [NCT01281735]), only 9% of children with CML who were treated with TKIs met the criteria for TKI discontinuation.[26] Other reports have also supported this trend.[27,28] Although the small number of children studied is a limitation, it appears that the outcome for TKI discontinuation in children with CML is similar to that of adults. Two of the larger pediatric studies that discuss this topic are summarized below:
- The Japan Pediatric Leukemia and Lymphoma Study Group (JPLSG) reported on 22 children with CML who met their criteria for TKI discontinuation, which was similar to the NCCN’s TKI discontinuation criteria.[28] The median age at CML diagnosis was 9 years, and the median age at TKI discontinuation was 16 years. The median duration of TKI therapy exceeded 8 years, and the median duration of MR4 before TKI discontinuation exceeded 4 years. Eleven of 22 children experienced loss of MMR at a median of 90 days after TKI discontinuation. All of these children subsequently regained MR4 after TKI resumption. The treatment-free remission rate at 12 months was 50%, and no relapses were observed beyond 4 months of TKI discontinuation.
TKI withdrawal syndrome is observed in approximately 20% to 30% of adults when TKI therapy is discontinued.[29] The syndrome includes musculoskeletal pain that typically develops within 2 months of TKI discontinuation and continues for several months. The JPLSG study did not observe musculoskeletal pain in children after TKI discontinuation.
- The International Registry of Childhood Chronic Myeloid Leukemia reported on 18 patients with CML who were younger than 18 years at diagnosis. These patients discontinued imatinib after meeting the criteria for TKI discontinuation (i.e., in chronic phase with a sustained DMR to imatinib [MR4; BCR::ABL1 transcript level ≤0.01% IS]) for at least 2 years.[26]
Among the 18 children who stopped taking imatinib, 9 (50%) eventually resumed treatment.[26] Seven of these nine patients experienced loss of MMR (BCR::ABL1 transcript level ≤0.1% IS). Six of the seven patients regained MR4 within a median of approximately 5 months after TKI reinitiation. The remaining patient achieved MMR after TKI reinitiation. Two additional patients who had a one-log increase in BCR::ABL1 transcript levels, but did not meet the criteria for loss of MMR, were restarted on imatinib by their physicians. For the other nine patients who remained in treatment-free remission, the median follow-up period after imatinib discontinuation was 50 months. TKI withdrawal syndrome was not reported in any patients discontinuing imatinib.
Treatment Options Under Clinical Evaluation
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, see the ClinicalTrials.gov website.
References
- Giona F, Putti MC, Micalizzi C, et al.: Long-term results of high-dose imatinib in children and adolescents with chronic myeloid leukaemia in chronic phase: the Italian experience. Br J Haematol 170 (3): 398-407, 2015. [PUBMED Abstract]
- Gore L, Kearns PR, de Martino ML, et al.: Dasatinib in Pediatric Patients With Chronic Myeloid Leukemia in Chronic Phase: Results From a Phase II Trial. J Clin Oncol 36 (13): 1330-1338, 2018. [PUBMED Abstract]
- Hijiya N, Maschan A, Rizzari C, et al.: Phase 2 study of nilotinib in pediatric patients with Philadelphia chromosome-positive chronic myeloid leukemia. Blood 134 (23): 2036-2045, 2019. [PUBMED Abstract]
- Brivio E, Pennesi E, Willemse ME, et al.: Bosutinib in Resistant and Intolerant Pediatric Patients With Chronic Phase Chronic Myeloid Leukemia: Results From the Phase I Part of Study ITCC054/COG AAML1921. J Clin Oncol 42 (7): 821-831, 2024. [PUBMED Abstract]
- Champagne MA, Capdeville R, Krailo M, et al.: Imatinib mesylate (STI571) for treatment of children with Philadelphia chromosome-positive leukemia: results from a Children’s Oncology Group phase 1 study. Blood 104 (9): 2655-60, 2004. [PUBMED Abstract]
- Millot F, Guilhot J, Nelken B, et al.: Imatinib mesylate is effective in children with chronic myelogenous leukemia in late chronic and advanced phase and in relapse after stem cell transplantation. Leukemia 20 (2): 187-92, 2006. [PUBMED Abstract]
- Millot F, Baruchel A, Guilhot J, et al.: Imatinib is effective in children with previously untreated chronic myelogenous leukemia in early chronic phase: results of the French national phase IV trial. J Clin Oncol 29 (20): 2827-32, 2011. [PUBMED Abstract]
- Champagne MA, Fu CH, Chang M, et al.: Higher dose imatinib for children with de novo chronic phase chronic myelogenous leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer 57 (1): 56-62, 2011. [PUBMED Abstract]
- Andolina JR, Neudorf SM, Corey SJ: How I treat childhood CML. Blood 119 (8): 1821-30, 2012. [PUBMED Abstract]
- Menon-Andersen D, Mondick JT, Jayaraman B, et al.: Population pharmacokinetics of imatinib mesylate and its metabolite in children and young adults. Cancer Chemother Pharmacol 63 (2): 229-38, 2009. [PUBMED Abstract]
- Millot F, Guilhot J, Baruchel A, et al.: Impact of early molecular response in children with chronic myeloid leukemia treated in the French Glivec phase 4 study. Blood 124 (15): 2408-10, 2014. [PUBMED Abstract]
- Hochhaus A, Baccarani M, Silver RT, et al.: European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia 34 (4): 966-984, 2020. [PUBMED Abstract]
- Shima H, Tokuyama M, Tanizawa A, et al.: Distinct impact of imatinib on growth at prepubertal and pubertal ages of children with chronic myeloid leukemia. J Pediatr 159 (4): 676-81, 2011. [PUBMED Abstract]
- Millot F, Guilhot J, Baruchel A, et al.: Growth deceleration in children treated with imatinib for chronic myeloid leukaemia. Eur J Cancer 50 (18): 3206-11, 2014. [PUBMED Abstract]
- Aplenc R, Blaney SM, Strauss LC, et al.: Pediatric phase I trial and pharmacokinetic study of dasatinib: a report from the children’s oncology group phase I consortium. J Clin Oncol 29 (7): 839-44, 2011. [PUBMED Abstract]
- Zwaan CM, Rizzari C, Mechinaud F, et al.: Dasatinib in children and adolescents with relapsed or refractory leukemia: results of the CA180-018 phase I dose-escalation study of the Innovative Therapies for Children with Cancer Consortium. J Clin Oncol 31 (19): 2460-8, 2013. [PUBMED Abstract]
- Novartis Pharmaceuticals Corporation: TASIGNA (nilotinib): Prescribing Information. East Hanover, NJ: Novartis, 2018. Available online. Last accessed April 7, 2022.
- O’Hare T, Shakespeare WC, Zhu X, et al.: AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell 16 (5): 401-12, 2009. [PUBMED Abstract]
- Cortes JE, Kim DW, Pinilla-Ibarz J, et al.: A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med 369 (19): 1783-96, 2013. [PUBMED Abstract]
- Prasad V, Mailankody S: The accelerated approval of oncologic drugs: lessons from ponatinib. JAMA 311 (4): 353-4, 2014 Jan 22-29. [PUBMED Abstract]
- Hughes TP, Mauro MJ, Cortes JE, et al.: Asciminib in Chronic Myeloid Leukemia after ABL Kinase Inhibitor Failure. N Engl J Med 381 (24): 2315-2326, 2019. [PUBMED Abstract]
- Réa D, Mauro MJ, Boquimpani C, et al.: A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood 138 (21): 2031-2041, 2021. [PUBMED Abstract]
- Hochhaus A, Wang J, Kim DW, et al.: Asciminib in Newly Diagnosed Chronic Myeloid Leukemia. N Engl J Med 391 (10): 885-898, 2024. [PUBMED Abstract]
- National Comprehensive Cancer Network: NCCN Guidelines for Patients: Chronic Myeloid Leukemia, 2021. Plymouth Meeting, PA: National Comprehensive Cancer Network, 2021. Available online with free subscription. Last accessed August 29, 2022.
- Dulucq S, Astrugue C, Etienne G, et al.: Risk of molecular recurrence after tyrosine kinase inhibitor discontinuation in chronic myeloid leukaemia patients: a systematic review of literature with a meta-analysis of studies over the last ten years. Br J Haematol 189 (3): 452-468, 2020. [PUBMED Abstract]
- Millot F, Suttorp M, Ragot S, et al.: Discontinuation of Imatinib in Children with Chronic Myeloid Leukemia: A Study from the International Registry of Childhood CML. Cancers (Basel) 13 (16): , 2021. [PUBMED Abstract]
- de Bruijn CMA, Millot F, Suttorp M, et al.: Discontinuation of imatinib in children with chronic myeloid leukaemia in sustained deep molecular remission: results of the STOP IMAPED study. Br J Haematol 185 (4): 718-724, 2019. [PUBMED Abstract]
- Shima H, Kada A, Tanizawa A, et al.: Discontinuation of tyrosine kinase inhibitors in pediatric chronic myeloid leukemia. Pediatr Blood Cancer 69 (8): e29699, 2022. [PUBMED Abstract]
- Berger MG, Pereira B, Rousselot P, et al.: Longer treatment duration and history of osteoarticular symptoms predispose to tyrosine kinase inhibitor withdrawal syndrome. Br J Haematol 187 (3): 337-346, 2019. [PUBMED Abstract]
Treatment of Recurrent or Refractory Childhood CML
Treatment options for children with recurrent or refractory chronic myeloid leukemia (CML) may include the following:
- Alternative tyrosine kinase inhibitor (TKI) therapy such as dasatinib, nilotinib, or bosutinib.
- Allogeneic hematopoietic stem cell transplant (HSCT).
Alternative TKI Therapy
In children who develop a hematologic or cytogenetic relapse during treatment with imatinib or who have an inadequate initial response to their initial TKI agents, determination of BCR::ABL1 kinase domain variant status should be considered to help guide subsequent therapy. Depending on the patient’s variant status, alternative TKIs such as dasatinib, nilotinib, or bosutinib can be considered on the basis of the adult and pediatric experience with these agents.[1–6]
Evidence (dasatinib in children with resistant or intolerant CML):
- In a study of 14 children with resistant or intolerant CML, the following results were observed:[6]
- 76% of patients were in complete cytogenetic remission, and 41% of patients had a major molecular response (MMR) after 12 months of dasatinib therapy.
- The progression-free survival (PFS) rate was 78% at 48 months.
Evidence (nilotinib in children with resistant or intolerant CML):
- In a study of 44 children with CML who were resistant or intolerant to imatinib or dasatinib, the following results were observed:[7]
- 40.7% of patients achieved an MMR after 12 months of nilotinib therapy.
- After a median of 11.3 months, no patients had experienced disease progression.
Dasatinib and nilotinib are active against many BCR::ABL1 variants that confer resistance to imatinib, although the agents are ineffective in patients with the T315I variant. In the presence of the T315I variant, which is resistant to all U.S. Food and Drug Administration (FDA)–approved TKIs, an allogeneic HSCT should be considered. Ponatinib, the BCR::ABL1 inhibitor effective against the T315I variant in adults, has not been prospectively studied in the pediatric population.
Allogeneic HSCT
The question of whether a pediatric patient with CML should receive an allogeneic HSCT when multiple TKIs are available remains unanswered. However, reports suggest that PFS does not improve when using HSCT, compared with the sustained use of imatinib.[8] The potential advantages and disadvantages need to be discussed with the patient and family. While HSCT is currently the only known definitive curative therapy for CML, patients discontinuing treatment with TKIs after sustained molecular remissions, who remained in molecular remission, have been reported.[9]
Treatment Options Under Clinical Evaluation
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, see the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- NCT04925479 (Study to Determine the Dose and Safety of Asciminib in Pediatric Patients With Chronic Myeloid Leukemia): This study aims to determine the dose and safety profile of asciminib in pediatric patients who were previously treated with one or more TKIs.
- NCT03934372 (An Open-Label, Single-Arm, Phase I/II Study Evaluating the Safety and Efficacy of Ponatinib for the Treatment of Recurrent or Refractory Leukemias, Lymphomas, or Solid Tumors in Pediatric Participants): This study will evaluate the safety, tolerability, pharmacokinetics, and efficacy of ponatinib in children aged 1 year to younger than 18 years.
References
- Hochhaus A, Baccarani M, Deininger M, et al.: Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia 22 (6): 1200-6, 2008. [PUBMED Abstract]
- le Coutre P, Ottmann OG, Giles F, et al.: Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is active in patients with imatinib-resistant or -intolerant accelerated-phase chronic myelogenous leukemia. Blood 111 (4): 1834-9, 2008. [PUBMED Abstract]
- Kantarjian H, O’Brien S, Talpaz M, et al.: Outcome of patients with Philadelphia chromosome-positive chronic myelogenous leukemia post-imatinib mesylate failure. Cancer 109 (8): 1556-60, 2007. [PUBMED Abstract]
- Kantarjian H, Shah NP, Hochhaus A, et al.: Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362 (24): 2260-70, 2010. [PUBMED Abstract]
- Saglio G, Kim DW, Issaragrisil S, et al.: Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 362 (24): 2251-9, 2010. [PUBMED Abstract]
- Gore L, Kearns PR, de Martino ML, et al.: Dasatinib in Pediatric Patients With Chronic Myeloid Leukemia in Chronic Phase: Results From a Phase II Trial. J Clin Oncol 36 (13): 1330-1338, 2018. [PUBMED Abstract]
- Novartis Pharmaceuticals Corporation: TASIGNA (nilotinib): Prescribing Information. East Hanover, NJ: Novartis, 2018. Available online. Last accessed April 7, 2022.
- Giona F, Putti MC, Micalizzi C, et al.: Long-term results of high-dose imatinib in children and adolescents with chronic myeloid leukaemia in chronic phase: the Italian experience. Br J Haematol 170 (3): 398-407, 2015. [PUBMED Abstract]
- Ross DM, Branford S, Seymour JF, et al.: Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 122 (4): 515-22, 2013. [PUBMED Abstract]
Latest Updates to This Summary (12/10/2024)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Treatment of Childhood Chronic Myeloid Leukemia (CML)
Added text to state that asciminib is an allosteric inhibitor of the myristoyl-binding pocket, whereas the previously described tyrosine kinase inhibitor (TKI) agents target the adenosine triphosphate (ATP)–binding pocket. Asciminib was initially used to treat adults with CML that had developed resistance to the ATP-binding pocket agents (cited Hughes et al. as reference 21). Asciminib was effective in this setting, and the U.S. Food and Drug Administration approved it to treat CML with the T315I variant (cited Réa et al. as reference 22). Subsequently, asciminib was approved to treat adults with newly diagnosed CML because major molecular response (MMR), as well as time to MMR, was significantly better with asciminib than with imatinib, and it trended similarly compared with second-generation TKIs. Safety profiles were also better with asciminib (cited Hochhaus et al. as reference 23). To date, there are no prospectively reported pediatric data for asciminib.
This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood chronic myeloid leukemia. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Childhood Chronic Myeloid Leukemia Treatment are:
- Alan Scott Gamis, MD, MPH (Children’s Mercy Hospital)
- Karen J. Marcus, MD, FACR (Dana-Farber of Boston Children’s Cancer Center and Blood Disorders Harvard Medical School)
- Jessica Pollard, MD (Dana-Farber/Boston Children’s Cancer and Blood Disorders Center)
- Michael A. Pulsipher, MD (Huntsman Cancer Institute at University of Utah)
- Rachel E. Rau, MD (University of Washington School of Medicine, Seatle Children’s)
- Lewis B. Silverman, MD (Dana-Farber Cancer Institute/Boston Children’s Hospital)
- Malcolm A. Smith, MD, PhD (National Cancer Institute)
- Sarah K. Tasian, MD (Children’s Hospital of Philadelphia)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website’s Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Chronic Myeloid Leukemia Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: /types/leukemia/hp/child-aml-treatment-pdq/childhood-cml-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 38630977]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
Based on the strength of the available evidence, treatment options may be described as either “standard” or “under clinical evaluation.” These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.