SUMMARY: The FDA on January 8, 2020, approved KEYTRUDA® (Pembrolizumab) for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, Non-Muscle Invasive Bladder Cancer (NMIBC) with Carcinoma In Situ (CIS) with or without papillary tumors, who are ineligible for or have elected not to undergo cystectomy.
The American Cancer Society estimates that for 2020, about 81,400 new cases of bladder cancer will be diagnosed in the US and about 17,980 patients will die of the disease. Bladder cancer is the fourth most common cancer in men, but is less common in women and the average age at the time of diagnosis is 73. Approximately 50% of all bladder cancers are non-invasive or in situ cancers. Patients with high-risk, Non-Muscle Invasive Bladder Cancer that has become unresponsive to BCG treatment, are often given the treatment option of radical cystectomy, which includes removing the entire urinary bladder and a prostatectomy for men or total hysterectomy in women. While highly curative, this surgical procedure carries substantial risk for morbidity and mortality, and can negatively impact patient’s quality of life. Further, a significant proportion of patients are medically ineligible for a radical cystectomy, and even if eligible, refuse surgery and opt for other less effective treatments, which could compromise outcomes.
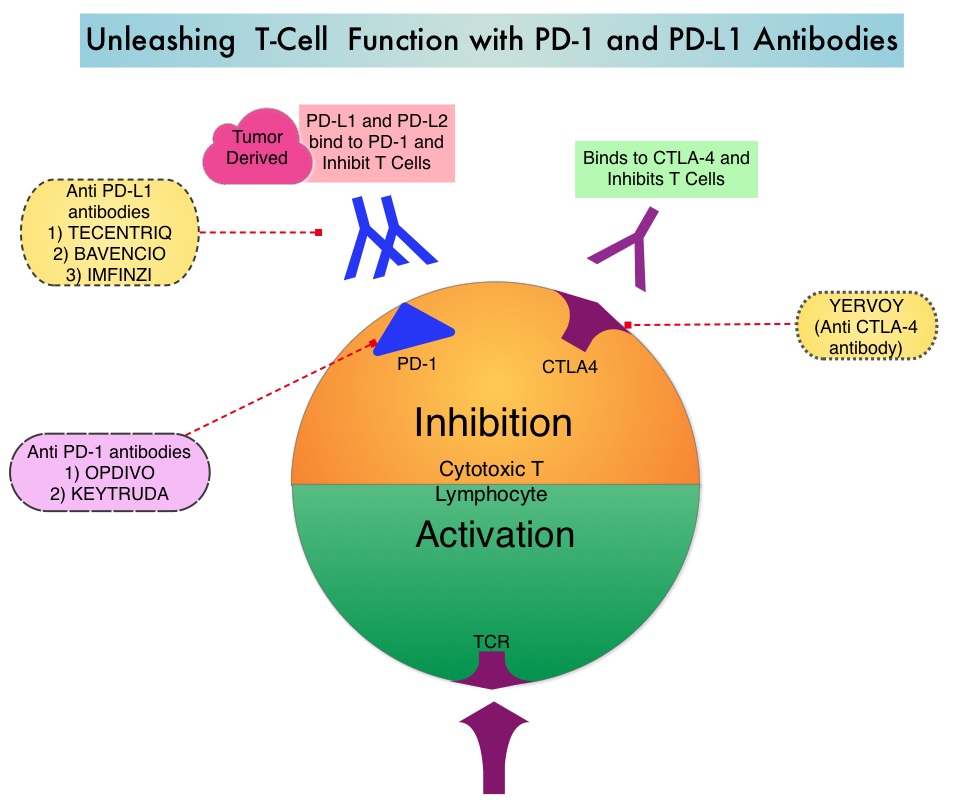
KEYTRUDA® is a fully humanized, Immunoglobulin G4, anti-PD-1, monoclonal antibody, that binds to the PD-1 receptor and blocks its interaction with ligands PD-L1 and PD-L2. By doing so, it unleashes the tumor-specific effector T cells, and is thereby able to undo PD-1 pathway-mediated inhibition of the immune response. KEYTRUDA® is presently approved by the FDA for the treatment of patients with locally advanced or metastatic Urothelial carcinoma who are not eligible for Cisplatin-containing chemotherapy or for those with disease progression during or following platinum-containing chemotherapy, based on its durable antitumor activity in this patient group. Upregulation of the PD-1 pathway has been observed in BCG-resistant NMIBC, suggesting that KEYTRUDA® may be of benefit in this group of patients.
This new FDA approval for KEYTRUDA® was based on the KEYNOTE-057 study, which is a multicenter, single-arm trial that enrolled 148 patients with high-risk NMIBC, of whom 96 patients had BCG-unresponsive CIS with or without papillary tumors. BCG-unresponsive high-risk Non-Muscle Invasive Bladder Cancer was defined as persistent disease despite adequate BCG therapy, disease recurrence after an initial tumor-free state following adequate BCG therapy, or T1 disease following a single induction course of BCG. Eligible patients had received adequate BCG therapy and were unable/unwilling to undergo radical cystectomy. All patients had undergone TransUrethral Resection of Bladder Tumor (TURBT) to remove resectable disease. Patients with residual Carcinoma In Situ, not amenable to complete resection were permitted. Patients received KEYTRUDA® 200 mg every 3 weeks until unacceptable toxicity, persistent or recurrent high-risk NMIBC or progressive disease, or up to 24 months of therapy without disease progression. The median age was 73 years and the median number of prior BCG instillations was 12. More than half of patients (56.9%) had a PD-L1 Combined Positive Score (CPS) of less than 10, and most patients in this analysis had refused prior cystectomy. The Primary end point was Complete Response Rate (CRR) as defined by negative results for cystoscopy with TURBT/biopsies as applicable, urine cytology, and CT Urography imaging. Secondary end points included Duration of Response and Safety.
At a median follow up was 28 months the Complete Response Rate was 41% and the median Duration of Response was 16.2 months. Forty-six percent (46%) of responding patients experienced a Complete Response lasting at least 12 months. The most frequent adverse reactions were fatigue, diarrhea, rash, pruritis, musculoskeletal pain, peripheral edema and hypothyroidism.
It was concluded from this study that KEYTRUDA® had encouraging activity in bladder cancer patients, with high-risk, BCG-unresponsive Carcinoma in Situ, with or without papillary tumors. The authors added that this study demonstrates that immune activation with systemically administered treatment can result in local activity in the bladder, as well as long-term durable remissions of cancer.
Keynote 057: Phase II trial of Pembrolizumab (pembro) for patients (pts) with high-risk (HR) nonmuscle invasive bladder cancer (NMIBC) unresponsive to bacillus calmette-guérin (BCG). Balar AV, Kulkarni GS, Uchio EM, et al. J Clin Oncol 37, 2019 (suppl 7S; abstr 350)