SUMMARY: The American Cancer Society estimates that for 2021, about 235,760 new cases of lung cancer will be diagnosed and 131,880 patients will die of the disease. Lung cancer is the leading cause of cancer-related mortality in the United States. Non-Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers. Of the three main subtypes of NSCLC, 30% are Squamous Cell Carcinomas (SCC), 40% are Adenocarcinomas and 10% are Large Cell Carcinomas. With changes in the cigarette composition and decline in tobacco consumption over the past several decades, Adenocarcinoma now is the most frequent histologic subtype of lung cancer.
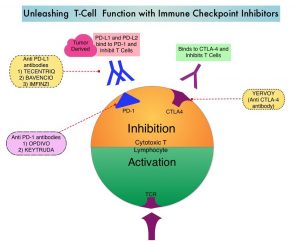
Patients with advanced NSCLC without a driver mutation and with Programmed cell Death Ligand 1 (PD-L1) expression of 50% or greater, are often treated first line with Immune Checkpoint Inhibition (ICI) monotherapy or ICI in combination with chemotherapy. The choice between these two treatment regimens is usually based on tumor burden and patient comorbidities, as there are presently no biomarkers available to predict the risk and benefit of these treatment interventions. The KEYNOTE-042 study demonstrated that single agent Pembrolizumab given as first line therapy demonstrated Overall Survival (OS) benefit over chemotherapy, in patients with previously untreated advanced NSCLC, with PD-L1 expression of 1% or greater. In an exploratory analysis, this benefit was seen regardless of KRAS status, but was more pronounced in patients with KRAS variants than those without KRAS variants.
The KRAS (kirsten rat sarcoma viral oncogene homologue) proto-oncogene encodes a protein that is a member of the small GTPase super family. The KRAS gene provides instructions for making the KRAS protein, which is a part of a signaling pathway known as the RAS/MAPK pathway. When mutated, KRAS oncogene has the potential to change normal cells cancerous. KRAS is the most frequently mutated oncogene in human cancers and are often associated with resistance to targeted therapies and poor outcomes. The KRAS-G12C mutation occurs in approximately 12-15% of NSCLC and in 3-5% of Colorectal cancers and other solid cancers. KRAS G12C is one of the most prevalent driver mutations in NSCLC and accounts for a greater number of patients than those with ALK, ROS1, RET, and TRK 1/2/3 mutations combined. KRAS G12C cancers are genomically more heterogeneous and occur more frequently in current or former smokers, and are likely to be more complex genomically than EGFR mutant or ALK rearranged cancers.
The authors conducted this study to evaluate the association of KRAS status with outcomes following ICI monotherapy versus chemoimmunotherapy in patients with PD-L1 of 50% or greater. The researchers used the Flatiron Health database, comprising 280 cancer clinics across the US and analyzed 1127 patients with advanced non-squamous NSCLC with PD-L1 expression of 50% or greater, known KRAS variant status, and no alteration in EGFR, ALK, or ROS1, who were treated with first line ICI monotherapy or chemoimmunotherapy between January 2016 and May 2020. Of the patients analyzed, 50.8% had KRAS variant status and 49.2% had KRAS wild type status. Patients with KRAS variant status were more likely to be female (58.7% versus 47.1%; P =0.002) and had smoking history (96.4% versus 87.7%; P < .001). Other patient demographics and patient characteristics, including age, race, ethnicity, Performance Status, and stage at diagnosis, were well balanced among the groups analyzed. Patient groups were stratified by treatment type and KRAS status (variant or wild type), and Overall Survival (OS) was compared between the treatment groups. Adjusted Hazard ratios for death associated with KRAS status and treatment regimen was estimated, using Cox proportional hazards models.
It was noted that among patients treated with ICI monotherapy, KRAS variant status was associated with superior median survival compared with KRAS wild type (21.1 months versus 13.6 months; HR=0.77; P=0.03), and this was statistically significant. However, among patients treated with chemoimmunotherapy, there was no significant median survival difference between patients with KRAS variant and KRAS wild type status (20.0 months versus 19.3 months; HR=0.99; P=0.93).
Among patients with KRAS variant status, the median OS did not differ between those treated with ICI monotherapy and chemoimmunotherapy (21.1 months versus 20.0 months; P =0.78), whereas among patients with KRAS wild type status, those treated with ICI monotherapy had numerically worse median survival than those treated with chemoimmunotherapy, although this difference was not statistically significant (13.6 months versus 19.3 months; HR=1.19; P =0.06).
In conclusion, this data suggests that chemoimmunotherapy might be favored over ICI monotherapy for patients with KRAS wild type tumors associated with high PD-L1 expression. The authors caution that in this analysis KRAS variant subtype and co-mutation status including TP53 and STK11 was unknown, and further investigation is needed to selection appropriate therapies for patients with PD-L1 High NSCLC.
Association Between KRAS Variant Status and Outcomes With First-line Immune Checkpoint Inhibitor–Based Therapy in Patients With Advanced Non–Small-Cell Lung Cancer. Sun L, Hsu M, Cohen RB, et al. JAMA Oncol. 2021;7:937-939.