Asbestos Exposure and Cancer Risk
What is asbestos?
Asbestos is the name given to six minerals that occur naturally in the environment as bundles of fibers that can be separated into thin, durable threads for use in commercial and industrial applications. These fibers are resistant to heat, fire, and chemicals and do not conduct electricity. For these reasons, asbestos has been used widely in many industries. Additional asbestos-like minerals are found in the natural environment, including erionite.
Chemically, asbestos minerals are silicate compounds, meaning they contain atoms of silicon and oxygen in their molecular structure.
Asbestos minerals are divided into two major groups: Serpentine asbestos and amphibole asbestos. Serpentine asbestos includes the mineral chrysotile, which has long, curly fibers that can be woven. Chrysotile asbestos is the form that has been used most widely in commercial applications. Amphibole asbestos includes the minerals actinolite, tremolite, anthophyllite, crocidolite, and amosite. Amphibole asbestos has straight, needle-like fibers that are more brittle than those of serpentine asbestos and are more limited in their ability to be fabricated (1, 2).
How is asbestos used?
Asbestos has been mined and used commercially in North America since the late 1800s. Its use increased greatly during World War II (3, 4). Since then, asbestos has been used in many industries. For example, the building and construction industries have used it for strengthening cement and plastics as well as for insulation, roofing, fireproofing, and sound absorption. The shipbuilding industry has used asbestos to insulate boilers, steam pipes, and hot water pipes. The automotive industry uses asbestos in vehicle brake shoes and clutch pads. Asbestos has also been used in ceiling and floor tiles; paints, coatings, and adhesives; and plastics. In addition, asbestos has been found in vermiculite-containing garden products and some talc-containing crayons.
In the late 1970s, the U.S. Consumer Product Safety Commission (CPSC) banned the use of asbestos in wallboard patching compounds and gas fireplaces because the asbestos fibers in these products could be released into the environment during use. In addition, manufacturers of electric hairdryers voluntarily stopped using asbestos in their products in 1979. In 1989, the U.S. Environmental Protection Agency (EPA) banned all new uses of asbestos; however, uses developed before 1989 are still allowed. The EPA also established regulations that require school systems to inspect buildings for the presence of damaged asbestos and to eliminate or reduce asbestos exposure to occupants by removing the asbestos or encasing it (2).
In June 2000, the CPSC concluded that the risk of children’s exposure to asbestos fibers in crayons was extremely low. U.S. manufacturers of these crayons agreed to eliminate talc from their products.
In August 2000, the EPA conducted a series of tests to evaluate the risk for consumers of adverse health effects associated with exposure to asbestos-contaminated vermiculite. The EPA concluded that exposure to asbestos from some vermiculite products poses only a minimal health risk. The EPA recommended that consumers reduce the low risk associated with the occasional use of vermiculite during gardening activities by limiting the amount of dust produced during vermiculite use. Specifically, the EPA suggested that consumers use vermiculite outdoors or in a well-ventilated area; keep vermiculite damp while using it; avoid bringing dust from vermiculite into the home on clothing; and use premixed potting soil, which is less likely to generate dust (2).
The regulations described above and other actions, coupled with widespread public concern about the health hazards of asbestos, have resulted in a significant annual decline in the U.S. use of asbestos. Domestic consumption of asbestos amounted to about 803,000 metric tons in 1973, but it had dropped to about 360 metric tons by 2015 (3, 5).
What are the health hazards of exposure to asbestos?
People may be exposed to asbestos in their workplace, their communities, or their homes. If products containing asbestos are disturbed, tiny asbestos fibers are released into the air. When asbestos fibers are breathed in, they may get trapped in the lungs and remain there for a long time. Over time, these fibers can accumulate and cause scarring and inflammation, which can affect breathing and lead to serious health problems (6).
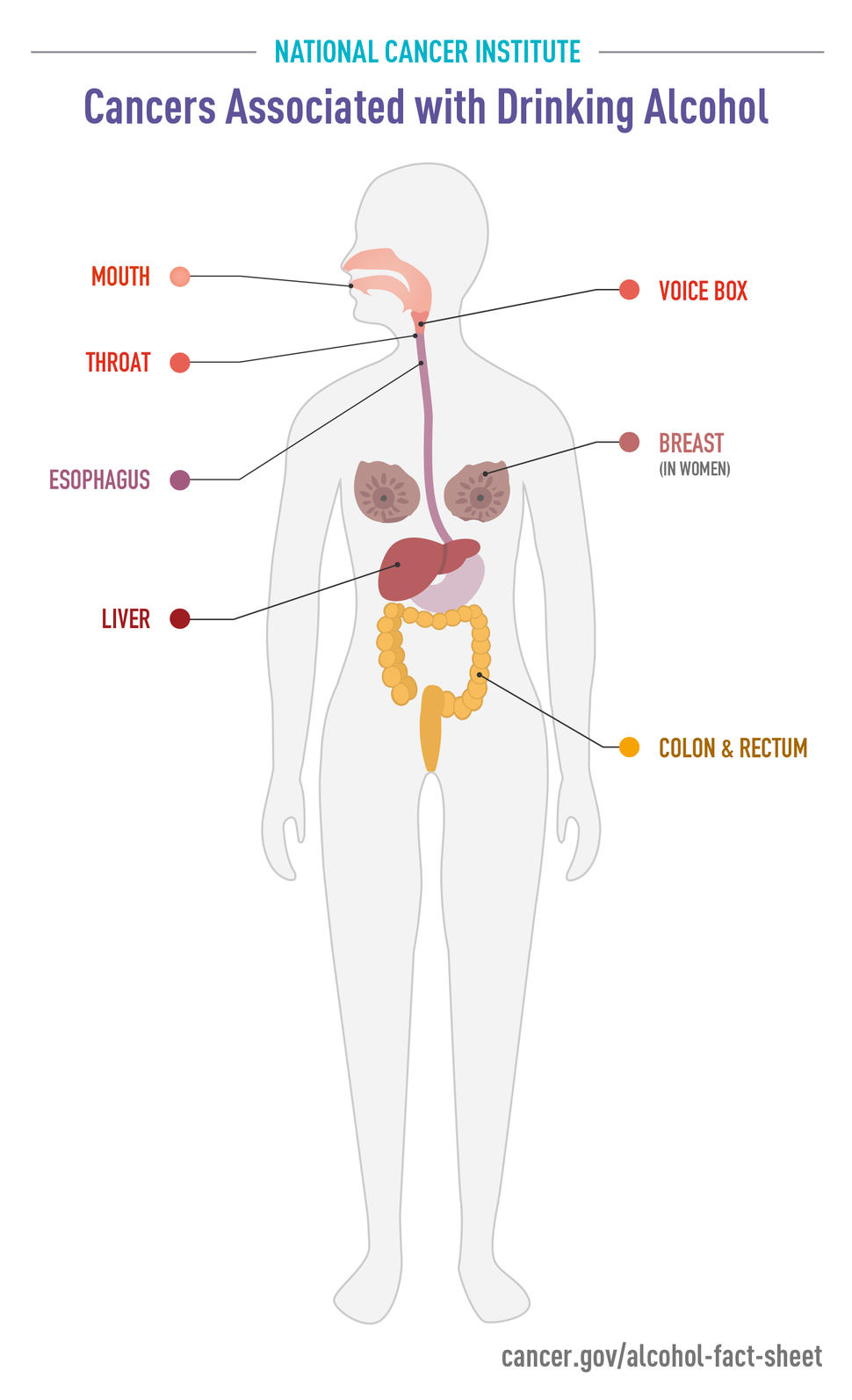
Asbestos has been classified as a known human carcinogen (a substance that causes cancer) by the U.S. Department of Health and Human Services (HHS), the U.S. Environmental Protection Agency (EPA), and the International Agency for Research on Cancer (IARC) (2, 3, 7, 8). According to IARC, there is sufficient evidence that asbestos causes mesothelioma (a relatively rare cancer of the thin membranes that line the chest and abdomen), and cancers of the lung, larynx, and ovary (8). In fact, it is thought that most mesotheliomas are due to asbestos exposure (9). There is limited evidence that asbestos exposure is linked to increased risks of cancers of the stomach, pharynx, and colorectum (8).
Asbestos exposure may also increase the risk of asbestosis (an inflammatory condition affecting the lungs that can cause shortness of breath, coughing, and permanent lung damage) and other nonmalignant lung and pleural disorders, including pleural plaques (changes in the membranes surrounding the lung), pleural thickening, and benign pleural effusions (abnormal collections of fluid between the thin layers of tissue lining the lungs and the wall of the chest cavity). Although pleural plaques are not precursors to lung cancer, evidence suggests that people with pleural disease caused by exposure to asbestos may be at increased risk for lung cancer (2, 10).
Erionite has also been classified as a known human carcinogen by IARC (8) and by HHS (3). It is not currently regulated by the EPA.
Who is at risk for an asbestos-related disease?
Everyone is exposed to asbestos at some time during their life. Low levels of asbestos are present in the air, water, and soil. However, most people do not become ill from their exposure. People who become ill from asbestos are usually those who are exposed to it on a regular basis, most often in a job where they work directly with the material or through substantial environmental contact.
Since the early 1940s, millions of American workers have been exposed to asbestos. Health hazards from asbestos fibers have been recognized in workers exposed in the shipbuilding trades, asbestos mining and milling, manufacturing of asbestos textiles and other asbestos products, insulation work in the construction and building trades, and a variety of other trades. Demolition workers, drywall removers, asbestos removal workers, firefighters, and automobile workers also may be exposed to asbestos fibers. Studies evaluating the cancer risk experienced by automobile mechanics exposed to asbestos through brake repair are limited, but the overall evidence suggests there is no safe level of asbestos exposure (3, 8). As a result of government regulations and improved work practices, today’s workers (those without previous exposure) are likely to face smaller risks than did those exposed in the past.
Individuals involved in the rescue, recovery, and cleanup at the site of the September 11, 2001, attacks on the World Trade Center (WTC) in New York City are another group at risk of developing an asbestos-related disease. Because asbestos was used in the construction of the North Tower of the WTC, when the building was attacked, hundreds of tons of asbestos were released into the atmosphere. Those at greatest risk include firefighters, police officers, paramedics, construction workers, and volunteers who worked in the rubble at Ground Zero. Others at risk include residents in close proximity to the WTC towers and those who attended schools nearby. These individuals will need to be followed to determine the long-term health consequences of their exposure (11). However, it is important to note that any symptoms these individuals experience may be related to exposure to debris components other than asbestos.
Although it is clear that the health risks from asbestos exposure increase with heavier exposure and longer exposure time, investigators have found asbestos-related diseases in individuals with only brief exposures. Generally, those who develop asbestos-related diseases show no signs of illness for a long time after exposure. It can take from 10 to 40 years or more for symptoms of an asbestos-related condition to appear (2).
There is some evidence that family members of workers heavily exposed to asbestos face an increased risk of developing mesothelioma (12). This risk is thought to result from exposure to asbestos fibers brought into the home on the shoes, clothing, skin, and hair of workers. To decrease these exposures, Federal law regulates workplace practices to limit the possibility of asbestos being brought home in this way. Some employees may be required to shower and change their clothes before they leave work, store their street clothes in a separate area of the workplace, or wash their work clothes at home separately from other clothes (2).
Cases of mesothelioma have also been seen in individuals without occupational asbestos exposure who live close to asbestos mines (12).
What factors affect the risk of developing an asbestos-related disease?
Several factors can help to determine how asbestos exposure affects an individual, including:
- Dose (how much asbestos an individual was exposed to)
- Duration (how long an individual was exposed)
- Size, shape, and chemical makeup of the asbestos fibers
- Source of the exposure
- Individual risk factors, such as smoking and pre-existing lung disease
- Genetic factors, such as having a germline mutation in BAP1 (13)
Although all forms of asbestos are considered hazardous, different types of asbestos fibers may be associated with different health risks. For example, the results of several studies suggest that amphibole forms of asbestos may be more harmful than chrysotile, particularly for mesothelioma risk, because they tend to stay in the lungs for a longer period of time (1, 2).
How does smoking affect risk?
Many studies have shown that the combination of smoking and asbestos exposure is particularly hazardous. Smokers who are also exposed to asbestos have a risk of developing lung cancer that is greater than the individual risks from asbestos and smoking added together (3, 6). There is evidence that quitting smoking will reduce the risk of lung cancer among asbestos-exposed workers (4). Smoking combined with asbestos exposure does not appear to increase the risk of mesothelioma (10). However, people who were exposed to asbestos on the job at any time during their life or who suspect they may have been exposed should not smoke.
How are asbestos-related diseases detected?
Individuals who have been exposed (or suspect they have been exposed) to asbestos fibers on the job, through the environment, or at home via a family contact should inform their doctor about their exposure history and whether or not they experience any symptoms. The symptoms of asbestos-related diseases may not become apparent for many decades after the exposure. It is particularly important to check with a doctor if any of the following symptoms develop:
- Shortness of breath, wheezing, or hoarseness
- A persistent cough that gets worse over time
- Blood in the sputum (fluid) coughed up from the lungs
- Pain or tightening in the chest
- Difficulty swallowing
- Swelling of the neck or face
- Loss of appetite
- Weight loss
- Fatigue or anemia
A thorough physical examination, including a chest x-ray and lung function tests, may be recommended. The chest x-ray is currently the most common tool used to detect asbestos-related diseases. Although chest x-rays cannot detect asbestos fibers in the lungs, they can help identify any early signs of lung disease resulting from asbestos exposure (2).
A lung biopsy, which detects microscopic asbestos fibers in pieces of lung tissue removed by surgery, is the most reliable test to confirm exposure to asbestos (2). A bronchoscopy is a less invasive test than a biopsy and detects asbestos fibers in material that is rinsed out of the lungs (2). It is important to note that these procedures cannot determine how much asbestos an individual may have been exposed to or whether disease will develop. Asbestos fibers can also be detected in urine, mucus, and feces, but these tests are not reliable for determining how much asbestos may be in an individual’s lungs (2).
How can workers protect themselves from asbestos exposure?
The Occupational Safety and Health Administration (OSHA) is a component of the U.S. Department of Labor (DOL) and is the Federal agency responsible for health and safety regulations in maritime, construction, manufacturing, and service workplaces. OSHA established regulations dealing with asbestos exposure on the job, specifically in construction work, shipyards, and general industry, that employers are required to follow. In addition, the Mine Safety and Health Administration (MSHA), another component of DOL, enforces regulations related to mine safety. Workers should use all protective equipment provided by their employers and follow recommended workplace practices and safety procedures. For example, National Institute for Occupational Safety and Health (NIOSH)-approved respirators that fit properly should be worn by workers when required.
Workers who are concerned about asbestos exposure in the workplace should discuss the situation with other employees, their employee health and safety representative, and their employers. If necessary, OSHA can provide more information or make an inspection. Information about regional offices can also be found on OSHA’s website at https://www.osha.gov/html/RAmap.html.
More information about asbestos is available on OSHA’s Asbestos page, which has links to information about asbestos in the workplace, including what OSHA standards apply, the hazards of asbestos, evaluating asbestos exposure, and controls used to protect workers. OSHA’s national office can be contacted at:
Office of Public Affairs
Occupational Safety and Health Administration
U.S. Department of Labor
202–693–1999
1–800–321–6742 (1–800–321–OSHA)
1–877–889–5627 (TTY)
https://www.osha.gov/workers (workers’ page)
Office of Public Affairs
Mine Safety and Health Administration
U.S. Department of Labor
202–693–9400
https://www.msha.gov
https://egov.msha.gov/HazardousConditionComplaint.aspx (Hazardous Condition Complaint)
The National Institute for Occupational Safety and Health (NIOSH), which is part of the Centers for Disease Control and Prevention (CDC), is another Federal agency that is concerned with asbestos exposure in the workplace. NIOSH conducts asbestos-related research, evaluates work sites for possible health hazards, and makes exposure control recommendations. In addition, NIOSH distributes publications on the health effects of asbestos exposure and can suggest additional sources of information. NIOSH can be contacted at:
Education and Information Division
Information Resources Branch
National Institute for Occupational Safety and Health
1–800–CDC–INFO (1–800–232–4636)
https://www.cdc.gov/niosh
What programs are available to help individuals with asbestos-related diseases?
Some people with asbestos-related illness may be eligible for Medicare coverage. Information about benefits is available from Medicare’s Regional Offices, located in 10 major cities across the United States and serving specific geographic areas. The Regional Offices serve as the agency’s initial point of contact for beneficiaries, health care providers, state and local governments, and the general public. General information about Medicare is available by calling toll-free 1–800–633–4227 (1–800–MEDICARE) or by visiting the Medicare website.
People with occupational asbestos-related diseases also may qualify for financial help, including medical payments, under state workers’ compensation laws. Because eligibility requirements vary from state to state, workers employed by private companies or by state and local government agencies should contact their state workers’ compensation board. Contact information for state workers’ compensation officials may be found at the U.S. Department of Labor (DOL) website.
If exposure occurred during employment with a Federal agency, medical expenses and other compensation may be covered by the Federal Employees’ Compensation Program, which is administered by the DOL Employment Standards Administration’s Office of Workers’ Compensation Programs. This program provides workers’ compensation benefits to Federal (civilian) employees for employment-related injuries and diseases. Benefits include wage replacement, payment for medical care, and, where necessary, medical and vocational rehabilitation assistance in returning to work. Benefits may also be provided to dependents if the injury or disease causes the employee’s death.
In addition, the Longshore and Harbor Workers’ Compensation Program provides benefits to longshoremen, harbor workers, other maritime workers, and other classes of private industry workers who are injured during the course of employment or suffer from diseases caused or worsened by conditions of employment. Information about eligibility and how to file a claim for benefits under either of these programs is available from:
Office of Workers’ Compensation Programs
Employment Standards Administration
U.S. Department of Labor
1–866–692–7487 (1–866–OWCPIVR)
202–693–0040 (Federal Employees’ Compensation Program)
202–693–0038 (Longshore and Harbor Workers’ Compensation Program)
https://www.dol.gov/agencies/owcp
Eligible veterans may receive health care at a Department of Veterans Affairs (VA) Medical Center for an asbestos-related disease. Veterans can receive treatment for service-connected and nonservice-connected medical conditions. Information about eligibility and benefits is available from the VA Health Benefits Service Center at 1–877–222–8387 (1–877–222–VETS) or on the VA website.
What other organizations offer information related to asbestos exposure?
The organizations listed below can provide more information about asbestos exposure.
The Agency for Toxic Substances and Disease Registry (ATSDR) is the principal Federal agency responsible for evaluating the human health effects of exposure to hazardous substances. This agency works in close collaboration with local, state, and other Federal agencies, with tribal governments, and with communities and local health care providers to help prevent or reduce harmful human health effects from exposure to hazardous substances. The ATSDR provides information about asbestos and where to find occupational and environmental health clinics. The ATSDR can be contacted at:
Agency for Toxic Substances and Disease Registry
1–800–232–4636 (1–800–CDC–INFO)
1–888–232–6348 (TTY)
https://www.atsdr.cdc.gov/
The U.S. Environmental Protection Agency (EPA) regulates the general public’s exposure to asbestos in buildings, drinking water, and the environment. The EPA offers a Toxic Substances Control Act (TSCA) Hotline and an Asbestos Ombudsman. The TSCA Hotline provides technical assistance and information about asbestos programs implemented under the TSCA, which include the Asbestos School Hazard Abatement Act and the Asbestos Hazard Emergency Response Act. The Asbestos Ombudsman focuses on asbestos in schools and handles questions and complaints. Both the TSCA Hotline and the Asbestos Ombudsman can provide publications on a number of topics, particularly on controlling asbestos exposure in schools and other buildings. The Ombudsman operates a toll-free hotline for small businesses, trade associations, and others seeking free, confidential help.
The EPA website includes a list of EPA state asbestos contacts. In addition, EPA’s Asbestos page provides links to information about asbestos and its health effects, including suggestions for homeowners who suspect asbestos in their homes, and laws and regulations applicable to asbestos. Questions may be directed to:
U.S. Environmental Protection Agency
202–554–1404 (TSCA Hotline)
1–800–368–5888 (Asbestos Ombudsman)
https://www.epa.gov/asbestos
Another EPA resource that may be of interest is the brochure titled Current Best Practices for Preventing Asbestos Exposure Among Brake and Clutch Repair Workers. Released in April 2007, this brochure includes work practices for both automotive professionals and home mechanics that may be used to avoid asbestos exposure. It also summarizes existing OSHA regulatory requirements for professional auto mechanics.
The U.S. Consumer Product Safety Commission (CPSC) is responsible for protecting the public from unreasonable risks of serious injury or death from more than 15,000 types of consumer products, including asbestos, under the agency’s jurisdiction. The CPSC maintains a toll-free 24-hour hotline where callers can obtain product safety and other agency information and report unsafe products. In addition, CPSC publications provide guidelines for repairing and removing asbestos, and general information about asbestos in the home. CPSC can be contacted at:
Office of Information and Public Affairs
U.S. Consumer Product Safety Commission
(301) 504-7923 (M-F 8 am – 4:30 pm ET)
1–800–638–2772 (Hotline)
301-595-7054 (TTY)
https://www.cpsc.gov/
Individuals can also contact their local or state health department with questions or concerns about asbestos.